Catatonia is a complex neuropsychiatric behavioral syndrome that is characterized by abnormal movements, immobility, abnormal behaviors, and withdrawal. The onset of catatonia can be acute or subtle and symptoms can wax, wane, or change during episodes. It has historically been related to schizophrenia, but catatonia is most often seen in mood disorders. It is now known that catatonic symptoms are nonspecific and may be observed in other mental, neurological, and medical conditions. Catatonia is now a stand-alone diagnosis, and the term is used to describe a feature of the underlying disorder.

Neurology is the branch of medicine dealing with the diagnosis and treatment of all categories of conditions and disease involving the nervous system, which comprises the brain, the spinal cord and the peripheral nerves. Neurological practice relies heavily on the field of neuroscience, the scientific study of the nervous system.
Cognitive neuropsychiatry is a growing multidisciplinary field arising out of cognitive psychology and neuropsychiatry that aims to understand mental illness and psychopathology in terms of models of normal psychological function. A concern with the neural substrates of impaired cognitive mechanisms links cognitive neuropsychiatry to the basic neuroscience. Alternatively, CNP provides a way of uncovering normal psychological processes by studying the effects of their change or impairment.
Biological psychiatry or biopsychiatry is an approach to psychiatry that aims to understand mental disorder in terms of the biological function of the nervous system. It is interdisciplinary in its approach and draws on sciences such as neuroscience, psychopharmacology, biochemistry, genetics, epigenetics and physiology to investigate the biological bases of behavior and psychopathology. Biopsychiatry is the branch of medicine which deals with the study of the biological function of the nervous system in mental disorders.
A monothematic delusion is a delusional state that concerns only one particular topic. This is contrasted by what is sometimes called multi-thematic or polythematic delusions where the person has a range of delusions. These disorders can occur within the context of schizophrenia or dementia or they can occur without any other signs of mental illness. When these disorders are found outside the context of mental illness, they are often caused by organic dysfunction as a result of traumatic brain injury, stroke, or neurological illness.
Clouding of consciousness, also called brain fog or mental fog, occurs when a person is slightly less wakeful or aware than normal. They are less aware of time and their surroundings, and find it difficult to pay attention. People describe this subjective sensation as their mind being "foggy".

Tourette syndrome is an inherited neurological disorder that begins in childhood or adolescence, characterized by the presence of multiple physical (motor) tics and at least one vocal (phonic) tic.
Child and adolescent psychiatry is a branch of psychiatry that focuses on the diagnosis, treatment, and prevention of mental disorders in children, adolescents, and their families. It investigates the biopsychosocial factors that influence the development and course of psychiatric disorders and treatment responses to various interventions. Child and adolescent psychiatrists primarily use psychotherapy and/or medication to treat mental disorders in the pediatric population.
Geriatric psychiatry, also known as geropsychiatry, psychogeriatrics or psychiatry of old age, is a branch of medicine and a subspecialty of psychiatry dealing with the study, prevention, and treatment of neurodegenerative, cognitive impairment, and mental disorders in people of old age. Geriatric psychiatry as a subspecialty has significant overlap with the specialties of geriatric medicine, behavioural neurology, neuropsychiatry, neurology, and general psychiatry. Geriatric psychiatry has become an official subspecialty of psychiatry with a defined curriculum of study and core competencies.
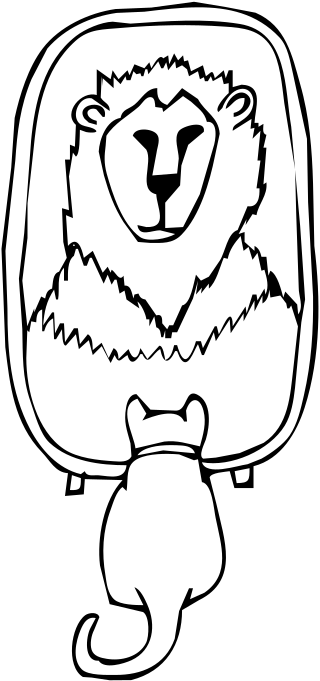
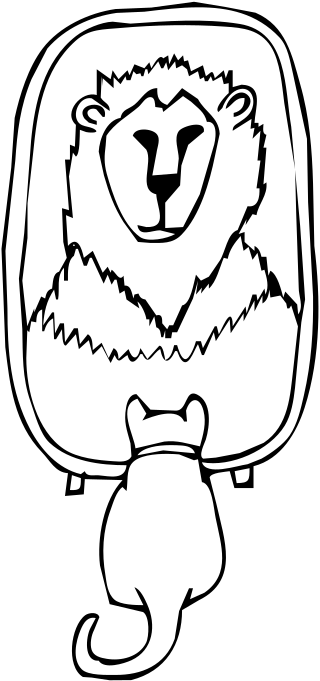
Grandiose delusions (GDs), also known as delusions of grandeur or expansive delusions, are a subtype of delusion characterized by extraordinary belief that one is famous, omnipotent, wealthy, or otherwise very powerful. Grandiose delusions often have a religious, science fictional, or supernatural theme. Examples include the extraordinary belief that one is a deity or celebrity, or that one possesses extraordinary talents, accomplishments, or superpowers.

Psychiatry is the medical specialty devoted to the diagnosis, prevention, and treatment of deleterious mental conditions. These include various matters related to mood, behaviour, cognition, perceptions, and emotions.
The Semel Institute for Neuroscience and Human Behavior is a research institute of the University of California Los Angeles (UCLA). It includes a number of centers, including the "Center for Neurobehavioral Genetics", which uses DNA sequencing, gene expression studies, bioinformatics, and the genetic manipulation of model organisms to understand brain and behavioral phenotypes.

Depression, one of the most commonly diagnosed psychiatric disorders, is being diagnosed in increasing numbers in various segments of the population worldwide. Depression in the United States alone affects 17.6 million Americans each year or 1 in 6 people. Depressed patients are at increased risk of type 2 diabetes, cardiovascular disease and suicide. Within the next twenty years depression is expected to become the second leading cause of disability worldwide and the leading cause in high-income nations, including the United States. In approximately 75% of suicides, the individuals had seen a physician within the prior year before their death, 45–66% within the prior month. About a third of those who died by suicide had contact with mental health services in the prior year, a fifth within the preceding month.
Clinical neuroscience is a branch of neuroscience that focuses on the scientific study of fundamental mechanisms that underlie diseases and disorders of the brain and central nervous system. It seeks to develop new ways of conceptualizing and diagnosing such disorders and ultimately of developing novel treatments.

The imprinted brain hypothesis is an unsubstantiated hypothesis in evolutionary psychology regarding the causes of autism spectrum and schizophrenia spectrum disorders, first presented by Bernard Crespi and Christopher Badcock in 2008. It claims that certain autistic and schizotypal traits are opposites, and that this implies the etiology of the two conditions must be at odds.
Perminder Sachdev is an Indian neuropsychiatrist based in Australia. He is a professor of neuropsychiatry at the University of New South Wales (UNSW), co-director of the UNSW Centre for Healthy Brain Aging, and clinical director of the Neuropsychiatric Institute at the Prince of Wales Hospital, Sydney. He is considered a trailblazer in the field of neuropsychiatry. Sachdev's research interests include ageing, vascular cognitive disorders such as vascular dementia, and psychiatric disorders.
The following outline is provided as an overview of and topical guide to psychiatry:
The American Neuropsychiatric Association (ANPA) is a non-profit organization of professionals in neuropsychiatry, behavioral neurology and the clinical neurosciences, with over 700 members from around the world. Established in 1988, its mission is to improve the lives of people with disorders at the interface of psychiatry and neurology, with the vision of transforming recognition, understanding and treatment of neuropsychiatric disorders. It founded in 1988 by two academic physicians doubly certified in neurology and psychiatry, Barry S. Fogel and Randolph Schiffer.

Barry S. Fogel is an American neuropsychiatrist, behavioral neurologist, medical writer, medical educator and inventor. He is the senior author of a standard text in neuropsychiatry and medical psychiatry, and a founder of the American Neuropsychiatric Association and the International Neuropsychiatric Association.
Carrie Elyse Bearden is an American psychologist and academic. She is a professor at the David Geffen School of Medicine, University of California, Los Angeles, and Director of the UCLA Center for the Assessment and Prevention of Prodromal States, a clinical research program for youth at high risk for psychotic disorders. She is most known for her research taking a ‘genetics first’ approach to study brain mechanisms underlying the development of serious mental illness. Her work has identified biological convergence between genetically and clinically defined high-risk populations.