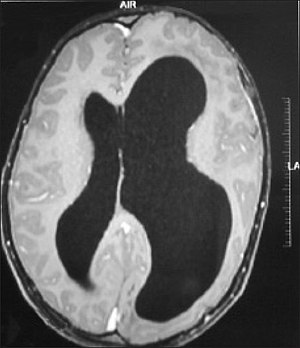
Colpocephaly is a cephalic disorder involving the disproportionate enlargement of the occipital horns of the lateral ventricles and is usually diagnosed early after birth due to seizures. It is a nonspecific finding and is associated with multiple neurological syndromes, including agenesis of the corpus callosum, Chiari malformation, lissencephaly, and microcephaly. Although the exact cause of colpocephaly is not known yet, it is commonly believed to occur as a result of neuronal migration disorders during early brain development, intrauterine disturbances, perinatal injuries, and other central nervous system disorders. Individuals with colpocephaly have various degrees of motor disabilities, visual defects, spasticity, and moderate to severe intellectual disability. No specific treatment for colpocephaly exists, but patients may undergo certain treatments to improve their motor function or intellectual disability.

Lissencephaly is a set of rare brain disorders whereby the whole or parts of the surface of the brain appear smooth. It is caused by defective neuronal migration during the 12th to 24th weeks of gestation resulting in a lack of development of brain folds (gyri) and grooves (sulci). It is a form of cephalic disorder. Terms such as agyria and pachygyria are used to describe the appearance of the surface of the brain.

Megalencephaly is a growth development disorder in which the brain is abnormally large. It is characterized by a brain with an average weight that is 2.5 standard deviations above the mean of the general population. Approximately 1 out of 50 children (2%) are said to have the characteristics of megalencephaly in the general population.

Focal cortical dysplasia (FCD) is a congenital abnormality of brain development where the neurons in an area of the brain failed to migrate in the proper formation in utero. Focal means that it is limited to a focal zone in any lobe. Focal cortical dysplasia is a common cause of intractable epilepsy in children and is a frequent cause of epilepsy in adults. There are three types of FCD with subtypes, including type 1a, 1b, 1c, 2a, 2b, 3a, 3b, 3c, and 3d, each with distinct histopathological features. All forms of focal cortical dysplasia lead to disorganization of the normal structure of the cerebral cortex :

Cerebellar hypoplasia is characterized by reduced cerebellar volume, even though cerebellar shape is (near) normal. It consists of a heterogeneous group of disorders of cerebellar maldevelopment presenting as early-onset non–progressive congenital ataxia, hypotonia and motor learning disability.

Alexander disease is a very rare autosomal dominant leukodystrophy, which are neurological conditions caused by anomalies in the myelin which protects nerve fibers in the brain. The most common type is the infantile form that usually begins during the first two years of life. Symptoms include mental and physical developmental delays, followed by the loss of developmental milestones, an abnormal increase in head size and seizures. The juvenile form of Alexander disease has an onset between the ages of 2 and 13 years. These children may have excessive vomiting, difficulty swallowing and speaking, poor coordination, and loss of motor control. Adult-onset forms of Alexander disease are less common. The symptoms sometimes mimic those of Parkinson’s disease or multiple sclerosis, or may present primarily as a psychiatric disorder.

Polymicrogyria (PMG) is a condition that affects the development of the human brain by multiple small gyri (microgyri) creating excessive folding of the brain leading to an abnormally thick cortex. This abnormality can affect either one region of the brain or multiple regions.

Neurofibromatosis type I (NF-1), or von Recklinghausen syndrome, is a complex multi-system human disorder caused by the mutation of Neurofibromin 1, a gene on chromosome 17 that is responsible for production of a protein which is needed for normal function in many human cell types. NF-1 causes tumors along the nervous system which can grow anywhere on the body. NF-1 is one of the most common genetic disorders and is not limited to any person's race or sex. NF-1 is an autosomal dominant disorder, which means that mutation or deletion of one copy of the NF-1 gene is sufficient for the development of NF-1, although presentation varies widely and is often different even between relatives affected by NF-1.

In neuroanatomy, a gyrus is a ridge on the cerebral cortex. It is generally surrounded by one or more sulci. Gyri and sulci create the folded appearance of the brain in humans and other mammals.

Sturge–Weber syndrome, sometimes referred to as encephalotrigeminal angiomatosis, is a rare congenital neurological and skin disorder. It is one of the phakomatoses and is often associated with port-wine stains of the face, glaucoma, seizures, intellectual disability, and ipsilateral leptomeningeal angioma. Sturge–Weber syndrome can be classified into three different types. Type 1 includes facial and leptomeningeal angiomas as well as the possibility of glaucoma or choroidal lesions. Normally, only one side of the brain is affected. This type is the most common. Type 2 involvement includes a facial angioma with a possibility of glaucoma developing. There is no evidence of brain involvement. Symptoms can show at any time beyond the initial diagnosis of the facial angioma. The symptoms can include glaucoma, cerebral blood flow abnormalities and headaches. More research is needed on this type of Sturge–Weber syndrome. Type 3 has leptomeningeal angioma involvement exclusively. The facial angioma is absent and glaucoma rarely occurs. This type is only diagnosed via brain scan.

In the field of neurology, temporal lobe epilepsy is an enduring brain disorder that causes unprovoked seizures from the temporal lobe. Temporal lobe epilepsy is the most common type of focal onset epilepsy among adults. Seizure symptoms and behavior distinguish seizures arising from the medial temporal lobe from seizures arising from the lateral (neocortical) temporal lobe. Memory and psychiatric comorbidities may occur. Diagnosis relies on electroencephalographic (EEG) and neuroimaging studies. Anticonvulsant medications, epilepsy surgery and dietary treatments may improve seizure control.
Pachygyria is a congenital malformation of the cerebral hemisphere. It results in unusually thick convolutions of the cerebral cortex. Typically, children have developmental delay and seizures, the onset and severity depending on the severity of the cortical malformation. Infantile spasms are common in affected children, as is intractable epilepsy.
Ohtahara syndrome (OS), also known as early infantile epileptic encephalopathy (EIEE) is a progressive epileptic encephalopathy. The syndrome is outwardly characterized by tonic spasms and partial seizures within the first few months of life, and receives its more elaborate name from the pattern of burst activity on an electroencephalogram (EEG). It is an extremely debilitating progressive neurological disorder, involving intractable seizures and severe intellectual disabilities. No single cause has been identified, although in many cases structural brain damage is present.

Macrocephaly-capillary malformation (M-CM) is a multiple malformation syndrome causing abnormal body and head overgrowth and cutaneous, vascular, neurologic, and limb abnormalities. Though not every patient has all features, commonly found signs include macrocephaly, congenital macrosomia, extensive cutaneous capillary malformation, body asymmetry, polydactyly or syndactyly of the hands and feet, lax joints, doughy skin, variable developmental delay and other neurologic problems such as seizures and low muscle tone.

Neuronal migration disorder (NMD) refers to a heterogenous group of disorders that, it is supposed, share the same etiopathological mechanism: a variable degree of disruption in the migration of neuroblasts during neurogenesis. The neuronal migration disorders are termed cerebral dysgenesis disorders, brain malformations caused by primary alterations during neurogenesis; on the other hand, brain malformations are highly diverse and refer to any insult to the brain during its formation and maturation due to intrinsic or extrinsic causes that ultimately will alter the normal brain anatomy. However, there is some controversy in the terminology because virtually any malformation will involve neuroblast migration, either primarily or secondarily.

Cavernous hemangioma, also called cavernous angioma, venous malformation, or cavernoma, is a type of venous malformation due to endothelial dysmorphogenesis from a lesion which is present at birth. A cavernoma in the brain is called a cerebral cavernous malformation or CCM. Despite its designation as a hemangioma, a cavernous hemangioma is not a tumor as it does not display endothelial hyperplasia. The abnormal tissue causes a slowing of blood flow through the cavities, or "caverns". The blood vessels do not form the necessary junctions with surrounding cells, and the structural support from the smooth muscle is hindered, causing leakage into the surrounding tissue. It is the leakage of blood, referred to as hemorrhage, that causes a variety of symptoms known to be associated with the condition.
Christopher A. Walsh is the Bullard Professor of Neurology at Harvard Medical School, Chief of the Division of Genetics at Children's Hospital Boston, Investigator of the Howard Hughes Medical Institute, and the former Director of the Harvard-MIT MD-PhD Program. His research focuses on genetics of human cortical development and somatic mutations contributions to human brain diseases.

Microlissencephaly (MLIS) is a rare congenital brain disorder that combines severe microcephaly with lissencephaly. Microlissencephaly is a heterogeneous disorder, i.e. it has many different causes and a variable clinical course. Microlissencephaly is a malformation of cortical development (MCD) that occurs due to failure of neuronal migration between the third and fifth month of gestation as well as stem cell population abnormalities. Numerous genes have been found to be associated with microlissencephaly, however, the pathophysiology is still not completely understood.
ZC4H2 is a protein-coding gene located on the X-chromosome. This gene encodes a protein which is a member of the so-called zinc finger domain-containing protein family. There is currently very limited understanding about the ZC4H2 gene and its protein function.

Muscle–eye–brain (MEB) disease, also known as muscular dystrophy-dystroglycanopathy congenital with brain and eye anomalies A3 (MDDGA3), is a kind of rare congenital muscular dystrophy (CMD), largely characterized by hypotonia at birth. Patients have muscular dystrophy, central nervous system abnormalities and ocular abnormalities. The condition is degenerative.