Lymphedema, also known as lymphoedema and lymphatic edema, is a condition of localized swelling caused by a compromised lymphatic system. The lymphatic system functions as a critical portion of the body's immune system and returns interstitial fluid to the bloodstream. Lymphedema is most frequently a complication of cancer treatment or parasitic infections, but it can also be seen in a number of genetic disorders. Though incurable and progressive, a number of treatments may improve symptoms. Tissues with lymphedema are at high risk of infection because the lymphatic system has been compromised.

Edema, also spelled oedema, and also known as fluid retention, dropsy, hydropsy and swelling, is the build-up of fluid in the body's tissue. Most commonly, the legs or arms are affected. Symptoms may include skin which feels tight, the area may feel heavy, and joint stiffness. Other symptoms depend on the underlying cause.

Respiratory failure results from inadequate gas exchange by the respiratory system, meaning that the arterial oxygen, carbon dioxide, or both cannot be kept at normal levels. A drop in the oxygen carried in the blood is known as hypoxemia; a rise in arterial carbon dioxide levels is called hypercapnia. Respiratory failure is classified as either Type 1 or Type 2, based on whether there is a high carbon dioxide level, and can be acute or chronic. In clinical trials, the definition of respiratory failure usually includes increased respiratory rate, abnormal blood gases, and evidence of increased work of breathing. Respiratory failure causes an altered mental status due to ischemia in the brain.

Heart failure (HF), also known as congestive heart failure (CHF), is a syndrome, a group of signs and symptoms, caused by an impairment of the heart's blood pumping function. Symptoms typically include shortness of breath, excessive fatigue, and leg swelling. The shortness of breath may occur with exertion or while lying down, and may wake people up during the night. Chest pain, including angina, is not usually caused by heart failure, but may occur if the heart failure was caused by a heart attack. The severity of the heart failure is mainly decided based on ejection fraction and also measured by the severity of symptoms. Other conditions that may have symptoms similar to heart failure include obesity, kidney failure, liver disease, anemia, and thyroid disease.

Fluid replacement or fluid resuscitation is the medical practice of replenishing bodily fluid lost through sweating, bleeding, fluid shifts or other pathologic processes. Fluids can be replaced with oral rehydration therapy (drinking), intravenous therapy, rectally such as with a Murphy drip, or by hypodermoclysis, the direct injection of fluid into the subcutaneous tissue. Fluids administered by the oral and hypodermic routes are absorbed more slowly than those given intravenously.

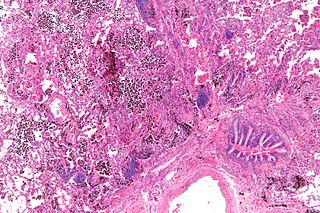
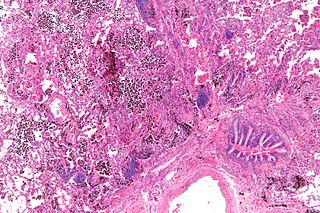
Pulmonary edema, also known as pulmonary congestion, is excessive liquid accumulation in the tissue and air spaces of the lungs. It leads to impaired gas exchange and may cause hypoxemia and respiratory failure. It is due to either failure of the left ventricle of the heart to remove oxygenated blood adequately from the pulmonary circulation, or an injury to the lung tissue directly or blood vessels of the lung.

Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Symptoms include shortness of breath (dyspnea), rapid breathing (tachypnea), and bluish skin coloration (cyanosis). For those who survive, a decreased quality of life is common.
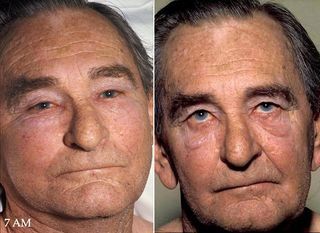
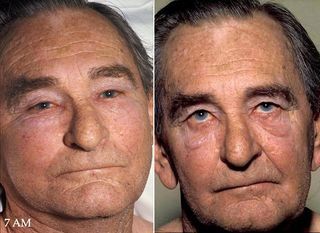
Superior vena cava syndrome (SVCS), is a group of symptoms caused by obstruction of the superior vena cava ("SVC"), a short, wide vessel carrying circulating blood into the heart. The majority of cases are caused by malignant tumors within the mediastinum, most commonly lung cancer and non-Hodgkin's lymphoma, directly compressing or invading the SVC wall. Non-malignant causes are increasing in prevalence due to expanding use of intravascular devices, which can result in thrombosis. Other non-malignant causes include benign mediastinal tumors, aortic aneurysm, infections, and fibrosing mediastinitis.
Pulmonary hemorrhage is an acute bleeding from the lung, from the upper respiratory tract and the trachea, and the pulmonary alveoli. When evident clinically, the condition is usually massive. The onset of pulmonary hemorrhage is characterized by a cough productive of blood (hemoptysis) and worsening of oxygenation leading to cyanosis. Treatment should be immediate and should include tracheal suction, oxygen, positive pressure ventilation, and correction of underlying abnormalities such as disorders of coagulation. A blood transfusion may be necessary.
Cardiac asthma is the medical condition of intermittent wheezing, coughing, and shortness of breath that is associated with underlying congestive heart failure (CHF). Symptoms of cardiac asthma are related to the heart's inability to effectively and efficiently pump blood in a CHF patient. This can lead to accumulation of fluid in and around the lungs, disrupting the lung's ability to oxygenate blood.

Respiratory diseases, or lung diseases, are pathological conditions affecting the organs and tissues that make gas exchange difficult in air-breathing animals. They include conditions of the respiratory tract including the trachea, bronchi, bronchioles, alveoli, pleurae, pleural cavity, the nerves and muscles of respiration. Respiratory diseases range from mild and self-limiting, such as the common cold, influenza, and pharyngitis to life-threatening diseases such as bacterial pneumonia, pulmonary embolism, tuberculosis, acute asthma, lung cancer, and severe acute respiratory syndromes, such as COVID-19. Respiratory diseases can be classified in many different ways, including by the organ or tissue involved, by the type and pattern of associated signs and symptoms, or by the cause of the disease.

Hypervolemia, also known as fluid overload, is the medical condition where there is too much fluid in the blood. The opposite condition is hypovolemia, which is too little fluid volume in the blood. Fluid volume excess in the intravascular compartment occurs due to an increase in total body sodium content and a consequent increase in extracellular body water. The mechanism usually stems from compromised regulatory mechanisms for sodium handling as seen in congestive heart failure (CHF), kidney failure, and liver failure. It may also be caused by excessive intake of sodium from foods, intravenous (IV) solutions and blood transfusions, medications, or diagnostic contrast dyes. Treatment typically includes administration of diuretics and limit the intake of water, fluids, sodium, and salt.

Alveolar lung diseases, are a group of diseases that mainly affect the alveoli of the lungs.

Smoke inhalation is the breathing in of harmful fumes through the respiratory tract. This can cause smoke inhalation injury which is damage to the respiratory tract caused by chemical and/or heat exposure, as well as possible systemic toxicity after smoke inhalation. Smoke inhalation can occur from fires of various sources such as residential, vehicle, and wildfires. Morbidity and mortality rates in fire victims with burns are increased in those with smoke inhalation injury. Victims of smoke inhalation injury can present with cough, difficulty breathing, low oxygen saturation, smoke debris and/or burns on the face. Smoke inhalation injury can affect the upper respiratory tract, usually due to heat exposure, or the lower respiratory tract, usually due to exposure to toxic fumes. Initial treatment includes taking the victim away from the fire and smoke, giving 100% oxygen at a high flow through a face mask, and checking the victim for injuries to the body. Treatment for smoke inhalation injury is largely supportive, with varying degrees of consensus on benefits of specific treatments.
Intraoperative blood salvage (IOS), also known as cell salvage, is a specific type of autologous blood transfusion. Specifically IOS is a medical procedure involving recovering blood lost during surgery and re-infusing it into the patient. It is a major form of autotransfusion.

Transfusion-related acute lung injury (TRALI) is the serious complication of transfusion of blood products that is characterized by the rapid onset of excess fluid in the lungs. It can cause dangerous drops in the supply of oxygen to body tissues. Although changes in transfusion practices have reduced the incidence of TRALI, it was the leading cause of transfusion-related deaths in the United States from fiscal year 2008 through fiscal year 2012.

Aquapheresis is a medical technology designed to remove excess salt and water from the body safely, predictably, and effectively from patients with a condition called fluid overload. It removes the excess salt and water and helps to restore a patient's proper fluid balance, which is called euvolemia.

A pulmonary contusion, also known as lung contusion, is a bruise of the lung, caused by chest trauma. As a result of damage to capillaries, blood and other fluids accumulate in the lung tissue. The excess fluid interferes with gas exchange, potentially leading to inadequate oxygen levels (hypoxia). Unlike pulmonary laceration, another type of lung injury, pulmonary contusion does not involve a cut or tear of the lung tissue.

Acute decompensated heart failure (ADHF) is a sudden worsening of the signs and symptoms of heart failure, which typically includes difficulty breathing (dyspnea), leg or feet swelling, and fatigue. ADHF is a common and potentially serious cause of acute respiratory distress. The condition is caused by severe congestion of multiple organs by fluid that is inadequately circulated by the failing heart. An attack of decompensation can be caused by underlying medical illness, such as myocardial infarction, an abnormal heart rhythm, infection, or thyroid disease.
Negative-pressure pulmonary edema (NPPE), also known as Postobstructive Pulmonary Edema, is a clinical phenomenon that results from the generation of large negative pressures in the airways during attempted inspiration against some form of obstruction of the upper airways. The most common reported cause of NPPE reported in adults is laryngospasm, while the most implicated causes in children are infectious croup and epiglottitis. The large negative pressures created in the airways by inhalation against an upper airway obstruction can lead to fluid being drawn from blood vessels supplying the lungs into the alveoli, causing pulmonary edema and impaired ability for oxygen exchange (hypoxemia). The main treatment for NPPE is supportive care in an intensive care unit and can be fatal without intervention.