Methadone, sold under the brand names Dolophine and Methadose among others, is a synthetic opioid agonist used for chronic pain and also for opioid use disorder. It is used to treat chronic pain, and it is also used to treat addiction to heroin or other opioids. Prescribed for daily use, the medicine relieves cravings and removes withdrawal symptoms. Withdrawal management using methadone can be accomplished in less than a month, or it may be done gradually over a longer period of time, or simply maintained for the rest of the patient's life. While a single dose has a rapid effect, maximum effect can take up to five days of use. After long-term use, in people with normal liver function, effects last 8 to 36 hours. Methadone is usually taken by mouth and rarely by injection into a muscle or vein.

Opioids are a class of drugs that derive from, or mimic, natural substances found in the opium poppy plant. Opioids work in the brain to produce a variety of effects, including pain relief. As a class of substances, they act on opioid receptors to produce morphine-like effects.

Opioid use disorder (OUD) is a substance use disorder characterized by cravings for opioids, continued use despite physical and/or psychological deterioration, increased tolerance with use, and withdrawal symptoms after discontinuing opioids. Opioid withdrawal symptoms include nausea, muscle aches, diarrhea, trouble sleeping, agitation, and a low mood. Addiction and dependence are important components of opioid use disorder.

Buprenorphine, sold under the brand name Subutex among others, is an opioid used to treat opioid use disorder, acute pain, and chronic pain. It can be used under the tongue (sublingual), in the cheek (buccal), by injection, as a skin patch (transdermal), or as an implant. For opioid use disorder, the patient must have moderate opioid withdrawal symptoms before buprenorphine can be administered under direct observation of a health-care provider.

Naltrexone, sold under the brand name Revia among others, is a medication primarily used to manage alcohol use or opioid use disorder by reducing cravings and feelings of euphoria associated with substance use disorder. It has also been found effective in the treatment of other addictions and may be used for them off-label. An opioid-dependent person should not receive naltrexone before detoxification. It is taken orally or by injection into a muscle. Effects begin within 30 minutes, though a decreased desire for opioids may take a few weeks to occur.
Physical dependence is a physical condition caused by chronic use of a tolerance-forming drug, in which abrupt or gradual drug withdrawal causes unpleasant physical symptoms. Physical dependence can develop from low-dose therapeutic use of certain medications such as benzodiazepines, opioids, stimulants, antiepileptics and antidepressants, as well as the recreational misuse of drugs such as alcohol, opioids and benzodiazepines. The higher the dose used, the greater the duration of use, and the earlier age use began are predictive of worsened physical dependence and thus more severe withdrawal syndromes. Acute withdrawal syndromes can last days, weeks or months. Protracted withdrawal syndrome, also known as post-acute-withdrawal syndrome or "PAWS", is a low-grade continuation of some of the symptoms of acute withdrawal, typically in a remitting-relapsing pattern, often resulting in relapse and prolonged disability of a degree to preclude the possibility of lawful employment. Protracted withdrawal syndrome can last for months, years, or depending on individual factors, indefinitely. Protracted withdrawal syndrome is noted to be most often caused by benzodiazepines. To dispel the popular misassociation with addiction, physical dependence to medications is sometimes compared to dependence on insulin by persons with diabetes.
Substance dependence, also known as drug dependence, is a biopsychological situation whereby an individual's functionality is dependent on the necessitated re-consumption of a psychoactive substance because of an adaptive state that has developed within the individual from psychoactive substance consumption that results in the experience of withdrawal and that necessitates the re-consumption of the drug. A drug addiction, a distinct concept from substance dependence, is defined as compulsive, out-of-control drug use, despite negative consequences. An addictive drug is a drug which is both rewarding and reinforcing. ΔFosB, a gene transcription factor, is now known to be a critical component and common factor in the development of virtually all forms of behavioral and drug addictions, but not dependence.
A methadone clinic is a medical facility where medications for opioid use disorder (MOUD) are dispensed-—historically and most commonly methadone, although buprenorphine is also increasingly prescribed. Medically assisted drug therapy treatment is indicated in patients who are opioid-dependent or have a history of opioid dependence. Methadone is a schedule II (USA) opioid analgesic, that is also prescribed for pain management. It is a long-acting opioid that can delay the opioid withdrawal symptoms that patients experience from taking short-acting opioids, like heroin, and allow time for withdrawal management. In the United States, by law, patients must receive methadone under the supervision of a physician, and dispensed through the Opioid Treatment Program (OTP) certified by the Substance Abuse and Mental Health Services Administration and registered with the Drug Enforcement Administration.

An opioid antagonist, or opioid receptor antagonist, is a receptor antagonist that acts on one or more of the opioid receptors.

Lefetamine (Santenol) is a drug which is a stimulant and also an analgesic with effects comparable to codeine.
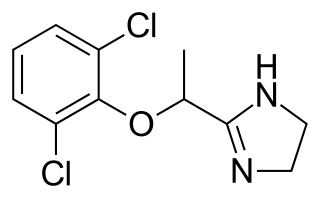
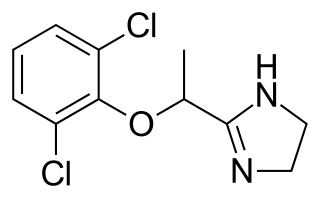
Lofexidine, sold under the brand name Lucemyra among others, is a medication historically used to treat high blood pressure; today, it is more commonly used to help with the physical symptoms of opioid withdrawal. It is taken by mouth. It is an α2A adrenergic receptor agonist. It was approved for use by the Food and Drug Administration in the United States in 2018.
Psychological dependence is a cognitive disorder and a form of dependence that is characterized by emotional–motivational withdrawal symptoms upon cessation of prolonged drug use or certain repetitive behaviors. Consistent and frequent exposure to particular substances or behaviors is responsible for inducing psychological dependence, requiring ongoing engagement to prevent the onset of an unpleasant withdrawal syndrome driven by negative reinforcement. Neuronal counter-adaptation is believed to contribute to the generation of withdrawal symptoms through changes in neurotransmitter activity or altered receptor expression. Environmental enrichment and physical activity have been shown to attenuate withdrawal symptoms.
Drug detoxification is variously construed or interpreted as a type of "medical" intervention or technique in regards to a physical dependence mediated by a drug; as well as the process and experience of a withdrawal syndrome or any of the treatments for acute drug overdose (toxidrome). The first definition however, in relation to substance dependence and its treatment is arguably a misnomer and even directly contradictory since withdrawal is neither contingent upon nor alleviated through biological excretion or clearance of the drug. In fact, excretion of a given drug from the body is one of the very processes that leads to withdrawal since the syndrome arises largely due to the cessation itself and the drug being absent from the body; especially the blood plasma, not from ‘leftover toxins’ or traces of the drug still being in the system.

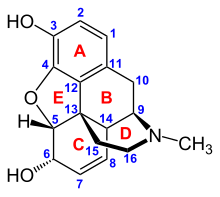
An opiate is an alkaloid substance derived from opium. It differs from the similar term opioid in that the latter is used to designate all substances, both natural and synthetic, that bind to opioid receptors in the brain. Opiates are alkaloid compounds naturally found in the opium poppy plant Papaver somniferum. The psychoactive compounds found in the opium plant include morphine, codeine, and thebaine. Opiates have long been used for a variety of medical conditions, with evidence of opiate trade and use for pain relief as early as the eighth century AD. Most opiates are considered drugs with moderate to high abuse potential and are listed on various "Substance-Control Schedules" under the Uniform Controlled Substances Act of the United States of America.
Neonatal withdrawal or neonatal abstinence syndrome (NAS) or neonatal opioid withdrawal syndrome (NOWS) is a withdrawal syndrome of infants, caused by the cessation of the administration of licit or illicit drugs. Tolerance, dependence, and withdrawal may occur as a result of repeated administration of drugs or even after short-term high-dose use—for example, during mechanical ventilation in intensive care units. There are two types of NAS: prenatal and postnatal. Prenatal NAS is caused by discontinuation of drugs taken by the pregnant mother, while postnatal NAS is caused by discontinuation of drugs directly to the infant.

Buprenorphine/naloxone, sold under the brand name Suboxone among others, is a fixed-dose combination medication that includes buprenorphine and naloxone. It is used to treat opioid use disorder, and reduces the mortality of opioid use disorder by 50%. It relieves cravings to use and withdrawal symptoms. Buprenorphine/naloxone is available for use in two different forms, under the tongue or in the cheek.

Harris Isbell was an American pharmacologist and the director of research for the NIMH Addiction Research Center at the Public Health Service Hospital in Lexington, Kentucky from 1945 to 1963. He did extensive research on the physical and psychological effects of various drugs on humans. Early work investigated aspects of physical dependence with opiates and barbiturates, while later work investigated psychedelic drugs, including LSD. The research was extensively reported in academic journals such as the Journal of Pharmacology and Experimental Therapeutics, Psychopharmacologia, and the AMA Archives of Neurology and Psychiatry.
Clinical Opiate Withdrawal Scale (COWS) is a method used by registered practitioners to measure the severity of a patient's opioid withdrawal symptoms. This method consists of a series of 11 topics each comprising 4 - 5 common symptoms experienced by a patient undergoing opioid withdrawal. In each topic a rank is given depending on what the patient responds to. Generally, 0 is considered to be no symptom shown and 4 or 5 is considered to be the most common and severe symptom shown. These results are then added up and a final diagnosis is made based on the value obtained. This test is crucial as it allows the practitioner to assess the physiological and psychological behaviours of the patient as well as the severity of each symptom during the duration of the examination. The results are grouped into 3 categories of mild, moderately severe and severe. Mild consists of 5 to 12 points, moderately severe consists of 13 to 24 points and anything above 36 points is severe and requires direct medical attention.

Opioid withdrawal is a set of symptoms arising from the sudden withdrawal or reduction of opioids where previous usage has been heavy and prolonged. Signs and symptoms of withdrawal can include drug craving, anxiety, restless legs, nausea, vomiting, diarrhea, sweating, and an increased heart rate. Opioid use triggers a rapid adaptation in cellular signalling pathways that means, when rapidly withdrawn, there can be adverse physiological effects. All opioids, both recreational drugs and medications, when reduced or stopped, can lead to opioid withdrawal symptoms. When withdrawal symptoms are due to recreational opioid use, the term opioid use disorder is used, whereas when due to prescribed medications, the term prescription opioid use disorder is used. Opioid withdrawal can be helped by the use of opioid replacement therapy, and symptoms may be relieved by the use of medications including lofexidine and clonidine.
Opioid agonist therapy (OAT) is a treatment in which prescribed opioid agonists are given to patients who live with Opioid use disorder (OUD). In the case of methadone maintenance treatment (MMT), methadone is used to treat dependence on heroin or other opioids, and is administered on an ongoing basis.