Cervix
Abnormal results include:[ citation needed ]
- Atypical squamous cells
- Atypical squamous cells of undetermined significance (ASC-US)
- Atypical squamous cells – cannot exclude HSIL (ASC-H)
- Low-grade squamous intraepithelial lesion (LGSIL or LSIL)
- High-grade squamous intraepithelial lesion (HGSIL or HSIL)
- Squamous cell carcinoma
- Atypical Glandular Cells not otherwise specified (AGC-NOS)
- Atypical Glandular Cells, suspicious for AIS or cancer (AGC-neoplastic)
- Adenocarcinoma in situ (AIS)
The results are calculated differently following a Pap smear of the cervix.[ citation needed ]
Squamous cell abnormalities
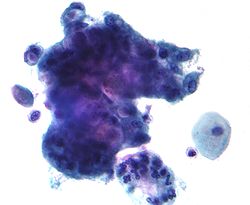
LSIL: low-grade squamous intraepithelial lesion

A low-grade squamous intraepithelial lesion (LSIL or LGSIL) indicates possible cervical dysplasia. LSIL usually indicates mild dysplasia (CIN 1), more than likely caused by a human papillomavirus infection. It is usually diagnosed following a Pap smear.[ citation needed ]
CIN 1 is the most common and most benign form of cervical intraepithelial neoplasia and usually resolves spontaneously within two years. Because of this, LSIL results can be managed with a simple "watch and wait" philosophy. However, because there is a 12–16% chance of progression to more severe dysplasia, the physician may want to follow the results more aggressively by performing a colposcopy with biopsy. [7] If the dysplasia progresses, treatment may be necessary. Treatment involves removal of the affected tissue, which can be accomplished by LEEP, cryosurgery, cone biopsy, or laser ablation.[ citation needed ]
HSIL: high-grade squamous intraepithelial lesion

High-grade squamous intraepithelial lesion (HSIL or HGSIL) indicates moderate or severe cervical intraepithelial neoplasia or carcinoma in situ. It is usually diagnosed following a Pap test. In some cases, these lesions can lead to invasive cervical cancer, if not followed appropriately.[ citation needed ]
HSIL does not mean that cancer is present. Of all women with HSIL results, 2% [8] or less [9] have invasive cervical cancer at that time; however, about 20% would progress to having invasive cervical cancer without treatment. [10] [ needs update ] To combat this progression, HSIL is usually followed by an immediate colposcopy with biopsy to sample or remove the dysplastic tissue. This tissue is sent for pathology testing to assign a histologic classification that is more definitive than a Pap smear result (which is a cytologic finding). HSIL generally corresponds to the histological classification of CIN 2 or 3.[ citation needed ]
HSIL treatment involves the removal or destruction of the affected cells, usually by LEEP. Other methods include cryotherapy, cautery, or laser ablation, but none are performed on pregnant women for fear of disrupting the pregnancy. [11] Any of these procedures is 85% likely to cure the problem.
Glandular cell abnormalities
Adenocarcinoma
Adenocarcinoma can arise from the endocervix, endometrium, and extrauterine sites.[ citation needed ]
AGC
AGC, formerly AGUS, is a term for atypical glandular cells of undetermined significance. [12] Renamed AGC to avoid confusion with ASCUS. [1]
The management of AGC is colposcopy with or without an endometrial biopsy.[ citation needed ]




