Jaundice, also known as icterus, is a yellowish or greenish pigmentation of the skin and sclera due to high bilirubin levels. Jaundice in adults is typically a sign indicating the presence of underlying diseases involving abnormal heme metabolism, liver dysfunction, or biliary-tract obstruction. The prevalence of jaundice in adults is rare, while jaundice in babies is common, with an estimated 80% affected during their first week of life. The most commonly associated symptoms of jaundice are itchiness, pale feces, and dark urine.

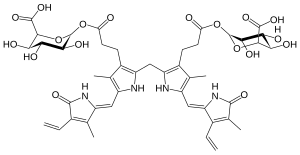
Bilirubin (BR) is a red-orange compound that occurs in the normal catabolic pathway that breaks down heme in vertebrates. This catabolism is a necessary process in the body's clearance of waste products that arise from the destruction of aged or abnormal red blood cells. In the first step of bilirubin synthesis, the heme molecule is stripped from the hemoglobin molecule. Heme then passes through various processes of porphyrin catabolism, which varies according to the region of the body in which the breakdown occurs. For example, the molecules excreted in the urine differ from those in the feces. The production of biliverdin from heme is the first major step in the catabolic pathway, after which the enzyme biliverdin reductase performs the second step, producing bilirubin from biliverdin.

Stercobilin is a tetrapyrrolic bile pigment and is one end-product of heme catabolism. It is the chemical responsible for the brown color of human feces and was originally isolated from feces in 1932. Stercobilin can be used as a marker for biochemical identification of fecal pollution levels in rivers.

A gallstone is a stone formed within the gallbladder from precipitated bile components. The term cholelithiasis may refer to the presence of gallstones or to any disease caused by gallstones, and choledocholithiasis refers to the presence of migrated gallstones within bile ducts.

Gilbert syndrome (GS) is a syndrome in which the liver of affected individuals processes bilirubin more slowly than the majority. Many people never have symptoms. Occasionally jaundice may occur.

Neonatal jaundice is a yellowish discoloration of the white part of the eyes and skin in a newborn baby due to high bilirubin levels. Other symptoms may include excess sleepiness or poor feeding. Complications may include seizures, cerebral palsy, or kernicterus.

Glucuronic acid is a uronic acid that was first isolated from urine. It is found in many gums such as gum arabic, xanthan, and kombucha tea and is important for the metabolism of microorganisms, plants and animals.
Cholestasis is a condition where the flow of bile from the liver to the duodenum is impaired. The two basic distinctions are:

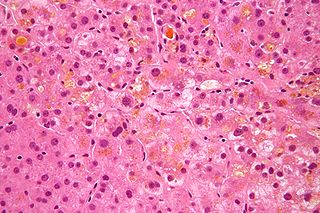
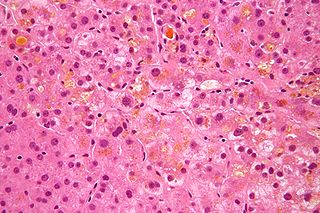
Dubin–Johnson syndrome is a rare, autosomal recessive, benign disorder that causes an isolated increase of conjugated bilirubin in the serum. Classically, the condition causes a black liver due to the deposition of a pigment similar to melanin. This condition is associated with a defect in the ability of hepatocytes to secrete conjugated bilirubin into the bile, and is similar to Rotor syndrome. It is usually asymptomatic, but may be diagnosed in early infancy based on laboratory tests. No treatment is usually needed.

Uridine 5'-diphospho-glucuronosyltransferase is a microsomal glycosyltransferase that catalyzes the transfer of the glucuronic acid component of UDP-glucuronic acid to a small hydrophobic molecule. This is a glucuronidation reaction.
The Model for End-Stage Liver Disease, or MELD, is a scoring system for assessing the severity of chronic liver disease. It was initially developed to predict mortality within three months of surgery in patients who had undergone a transjugular intrahepatic portosystemic shunt (TIPS) procedure, and was subsequently found to be useful in determining prognosis and prioritizing for receipt of a liver transplant. This score is now used by the United Network for Organ Sharing (UNOS) and Eurotransplant for prioritizing allocation of liver transplants instead of the older Child-Pugh score.
Probable phospholipid-transporting ATPase IC is an enzyme that in humans is encoded by the ATP8B1 gene. This protein is associated with progressive familial intrahepatic cholestasis type 1 as well as benign recurrent intrahepatic cholestasis.
In enzymology, a bilirubin-glucuronoside glucuronosyltransferase is an enzyme that catalyzes the chemical reaction

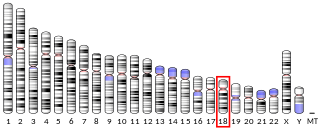
Multidrug resistance-associated protein 2 (MRP2) also called canalicular multispecific organic anion transporter 1 (cMOAT) or ATP-binding cassette sub-family C member 2 (ABCC2) is a protein that in humans is encoded by the ABCC2 gene.

UDP-glucuronosyltransferase 1-6 is an enzyme that in humans is encoded by the UGT1A6 gene.
The Lille Model is a medical modeling tool for predicting mortality in patients with alcoholic hepatitis who are not responding to steroid therapy. The model risk stratifies patients who have been receiving steroid treatment for seven days to predict who will improve and who should be considered for alternative treatment options including early referral for transplant.

Estradiol glucuronide, or estradiol 17β-D-glucuronide, is a conjugated metabolite of estradiol. It is formed from estradiol in the liver by UDP-glucuronyltransferase via attachment of glucuronic acid and is eventually excreted in the urine by the kidneys. It has much higher water solubility than does estradiol. Glucuronides are the most abundant estrogen conjugates.

Bilirubin glucuronide is a water-soluble reaction intermediate over the process of conjugation of indirect bilirubin. Bilirubin glucuronide itself belongs to the category of conjugated bilirubin along with bilirubin di-glucuronide. However, only the latter one is primarily excreted into the bile in the normal setting.
Hemolytic jaundice, also known as prehepatic jaundice, is a type of jaundice arising from hemolysis or excessive destruction of red blood cells, when the byproduct bilirubin is not excreted by the hepatic cells quickly enough. Unless the patient is concurrently affected by hepatic dysfunctions or is experiencing hepatocellular damage, the liver does not contribute to this type of jaundice.
Hyperbilirubinemia is a clinical condition describing an elevation of blood bilirubin level due to the inability to properly metabolise or excrete bilirubin, a product of erythrocytes breakdown. In severe cases, it is manifested as jaundice, the yellowing of tissues like skin and the sclera when excess bilirubin deposits in them. The US records 52,500 jaundice patients annually. By definition, bilirubin concentration of greater than 3 mg/ml is considered hyperbilirubinemia, following which jaundice progressively develops and becomes apparent when plasma levels reach 20 mg/ml. Rather than a disease itself, hyperbilirubinemia is indicative of multifactorial underlying disorders that trace back to deviations from regular bilirubin metabolism. Diagnosis of hyperbilirubinemia depends on physical examination, urinalysis, serum tests, medical history and imaging to identify the cause. Genetic diseases, alcohol, pregnancy and hepatitis viruses affect the likelihood of hyperbilirubinemia. Causes of hyperbilirubinemia mainly arise from the liver. These include haemolytic anaemias, enzymatic disorders, liver damage and gallstones. Hyperbilirubinemia itself is often benign. Only in extreme cases does kernicterus, a type of brain injury, occur. Therapy for adult hyperbilirubinemia targets the underlying diseases but patients with jaundice often have poor outcomes.