Ameloblastoma is a rare, benign or cancerous tumor of odontogenic epithelium much more commonly appearing in the lower jaw than the upper jaw. It was recognized in 1827 by Cusack. This type of odontogenic neoplasm was designated as an adamantinoma in 1885 by the French physician Louis-Charles Malassez. It was finally renamed to the modern name ameloblastoma in 1930 by Ivey and Churchill.

The dental follicle, also known as dental sac, is made up of mesenchymal cells and fibres surrounding the enamel organ and dental papilla of a developing tooth. It is a vascular fibrous sac containing the developing tooth and its odontogenic organ. The dental follicle (DF) differentiates into the periodontal ligament. In addition, it may be the precursor of other cells of the periodontium, including osteoblasts, cementoblasts and fibroblasts. They develop into the alveolar bone, the cementum with Sharpey's fibers and the periodontal ligament fibers respectively. Similar to dental papilla, the dental follicle provides nutrition to the enamel organ and dental papilla and also have an extremely rich blood supply.

Cherubism is a rare genetic disorder that causes prominence in the lower portion in the face. The name is derived from the temporary chubby-cheeked resemblance to putti, the chubby-faced infants featured in Renaissance paintings, which were often mistakenly described as cherubs.
Epulis fissuratum is a benign hyperplasia of fibrous connective tissue which develops as a reactive lesion to chronic mechanical irritation produced by the flange of a poorly fitting denture. More simply, epulis fissuratum is where excess folds of firm tissue form inside the mouth, as a result of rubbing on the edge of dentures that do not fit well. It is a harmless condition and does not represent oral cancer. Treatment is by simple surgical removal of the lesion, and also by adjustment of the denture or provision of a new denture.
An oral medicine or stomatology doctor/dentist has received additional specialized training and experience in the diagnosis and management of oral mucosal abnormalities including oral cancer, salivary gland disorders, temporomandibular disorders and facial pain, taste and smell disorders; and recognition of the oral manifestations of systemic and infectious diseases. It lies at the interface between medicine and dentistry. An oral medicine doctor is trained to diagnose and manage patients with disorders of the orofacial region.

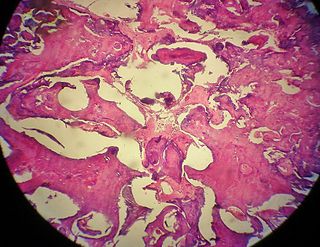
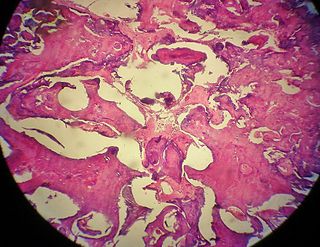
A dentigerous cyst, also known as a follicular cyst, is an epithelial-lined developmental cyst formed by accumulation of fluid between the reduced enamel epithelium and the crown of an unerupted tooth. It is formed when there is an alteration in the reduced enamel epithelium and encloses the crown of an unerupted tooth at the cemento-enamel junction. Fluid is accumulated between reduced enamel epithelium and the crown of an unerupted tooth.
Giant-cell fibroma is a benign localized fibrous mass. It often mimics other fibroepithelial growths and can be distinguished by its histopathology. The exact cause of giant-cell fibromas is unknown however there is no evidence to show that it can be caused by irritation. Giant-cell fibromas can be removed by surgical incision, electrosurgery, or laser excision.

An odontogenic keratocyst is a rare and benign but locally aggressive developmental cyst. It most often affects the posterior mandible and most commonly presents in the third decade of life. Odontogenic keratocysts make up around 19% of jaw cysts. Despite its more common appearance in the bone region, it can affect soft tissue.

Calcifying odontogenic cyst (COC) is a rare developmental lesion that comes from odontogenic epithelium. It is also known as a calcifying cystic odontogenic tumor, which is a proliferation of odontogenic epithelium and scattered nest of ghost cells and calcifications that may form the lining of a cyst, or present as a solid mass.

A glandular odontogenic cyst (GOC) is a rare and usually benign odontogenic cyst developed at the odontogenic epithelium of the mandible or maxilla. Originally, the cyst was labeled as "sialo-odontogenic cyst" in 1987. However, the World Health Organization (WHO) decided to adopt the medical expression "glandular odontogenic cyst". Following the initial classification, only 60 medically documented cases were present in the population by 2003. GOC was established as its own biological growth after differentiation from other jaw cysts such as the "central mucoepidermoid carcinoma (MEC)", a popular type of neoplasm at the salivary glands. GOC is usually misdiagnosed with other lesions developed at the glandular and salivary gland due to the shared clinical signs. The presence of osteodentin supports the concept of an odontogenic pathway. This odontogenic cyst is commonly described to be a slow and aggressive development. The inclination of GOC to be large and multilocular is associated with a greater chance of remission. GOC is an infrequent manifestation with a 0.2% diagnosis in jaw lesion cases. Reported cases show that GOC mainly impacts the mandible and male individuals. The presentation of GOC at the maxilla has a very low rate of incidence. The GOC development is more common in adults in their fifth and sixth decades.

An ameloblastic fibroma is a fibroma of the ameloblastic tissue, that is, an odontogenic tumor arising from the enamel organ or dental lamina. It may be either truly neoplastic or merely hamartomatous. In neoplastic cases, it may be labeled an ameloblastic fibrosarcoma in accord with the terminological distinction that reserves the word fibroma for benign tumors and assigns the word fibrosarcoma to malignant ones. It is more common in the first and second decades of life, when odontogenesis is ongoing, than in later decades. In 50% of cases an unerupted tooth is involved.
An odontoma, also known as an odontome, is a benign tumour linked to tooth development. Specifically, it is a dental hamartoma, meaning that it is composed of normal dental tissue that has grown in an irregular way. It includes both odontogenic hard and soft tissues. As with normal tooth development, odontomas stop growing once mature which makes them benign.
Peripheral odontogenic fibroma(PFO) is a fibrous connective tissue mass that is exophytic and covered in surface epithelium that contains odontogenic epithelium. The World Health Organization (WHO) classifies peripheral odontogenic fibroma as a fibroblastic neoplasm with variable amounts of odontogenic epithelium that appears to be dormant. Dentine and/or cementum-like material may be present.
The odontogenic myxoma is an uncommon benign odontogenic tumor arising from embryonic connective tissue associated with tooth formation. As a myxoma, this tumor consists mainly of spindle shaped cells and scattered collagen fibers distributed through a loose, mucoid material.
The calcifying epithelial odontogenic tumor (CEOT), also known as a Pindborg tumor, is an odontogenic tumor first recognized by the Danish pathologist Jens Jørgen Pindborg in 1955. It was previously described as an adenoid adamantoblastoma, unusual ameloblastoma and a cystic odontoma. Like other odontogenic neoplasms, it is thought to arise from the epithelial element of the enamel origin. It is a typically benign and slow growing, but invasive neoplasm.

The brown tumor is a bone lesion that arises in settings of excess osteoclast activity, such as hyperparathyroidism. They are a form of osteitis fibrosa cystica. It is not a neoplasm, but rather simply a mass. It most commonly affects the maxilla and mandible, though any bone may be affected. Brown tumours are radiolucent on x-ray.
Epulis is any tumor-like enlargement situated on the gingival or alveolar mucosa. The word literally means "(growth) on the gingiva", and describes only the location of the mass and has no further implications on the nature of the lesion. There are three types: fibromatous, ossifying and acanthomatous. The related term parulis refers to a mass of inflamed granulation tissue at the opening of a draining sinus on the alveolus over the root of an infected tooth. Another closely related term is gingival enlargement, which tends to be used where the enlargement is more generalized over the whole gingiva rather than a localized mass.
Odontogenic cysts are a group of jaw cysts that are formed from tissues involved in odontogenesis. Odontogenic cysts are closed sacs, and have a distinct membrane derived from the rest of odontogenic epithelium. It may contain air, fluids, or semi-solid material. Intra-bony cysts are most common in the jaws, because the mandible and maxilla are the only bones with epithelial components. That odontogenic epithelium is critical in normal tooth development. However, epithelial rests may be the origin for the cyst lining later. Not all oral cysts are odontogenic cysts. For example, mucous cyst of the oral mucosa and nasolabial duct cyst are not of odontogenic origin.
Cysts of the jaws are cysts—pathological epithelial-lined cavities filled with fluid or soft material—occurring on the bones of the jaws, the mandible and maxilla. Those are the bones with the highest prevalence of cysts in the human body, due to the abundant amount of epithelial remnants that can be left in the bones of the jaws. The enamel of teeth is formed from ectoderm, and so remnants of epithelium can be left in the bone during odontogenesis. The bones of the jaws develop from embryologic processes which fuse, and ectodermal tissue may be trapped along the lines of this fusion. This "resting" epithelium is usually dormant or undergoes atrophy, but, when stimulated, may form a cyst. The reasons why resting epithelium may proliferate and undergo cystic transformation are generally unknown, but inflammation is thought to be a major factor. The high prevalence of tooth impactions and dental infections that occur in the bones of the jaws is also significant to explain why cysts are more common at these sites.
The ameloblastic fibro-odontoma (AFO) is essentially a benign tumor with the features characteristic of ameloblastic fibroma along with enamel and dentin. Though it is generally regarded as benign, there have been cases of its malignant transformation into ameloblastic fibrosarcoma and odontogenic sarcoma. Cahn LR and Blum T, believed in "maturation theory", which suggested that AFO was an intermediate stage and eventually developed during the period of tooth formation to a complex odontoma thus, being a hamartoma.