Haematopoiesis is the formation of blood cellular components. All cellular blood components are derived from haematopoietic stem cells. In a healthy adult human, roughly ten billion to a hundred billion new blood cells are produced per day, in order to maintain steady state levels in the peripheral circulation.

Giant cell arteritis (GCA), also called temporal arteritis, is an inflammatory autoimmune disease of large blood vessels. Symptoms may include headache, pain over the temples, flu-like symptoms, double vision, and difficulty opening the mouth. Complications can include blockage of the artery to the eye with resulting blindness, as well as aortic dissection, and aortic aneurysm. GCA is frequently associated with polymyalgia rheumatica. It can be confirmed by biopsy of the temporal artery in about 90% of people.

A granuloma is an aggregation of macrophages that forms in response to chronic inflammation. This occurs when the immune system attempts to isolate foreign substances that it is otherwise unable to eliminate. Such substances include infectious organisms including bacteria and fungi, as well as other materials such as foreign objects, keratin, and suture fragments.
A syncytium or symplasm is a multinucleate cell that can result from multiple cell fusions of uninuclear cells, in contrast to a coenocyte, which can result from multiple nuclear divisions without accompanying cytokinesis. The muscle cell that makes up animal skeletal muscle is a classic example of a syncytium cell. The term may also refer to cells interconnected by specialized membranes with gap junctions, as seen in the heart muscle cells and certain smooth muscle cells, which are synchronized electrically in an action potential.

An osteoclast is a type of bone cell that breaks down bone tissue. This function is critical in the maintenance, repair, and remodeling of bones of the vertebral skeleton. The osteoclast disassembles and digests the composite of hydrated protein and mineral at a molecular level by secreting acid and a collagenase, a process known as bone resorption. This process also helps regulate the level of blood calcium.

Polymyalgia rheumatica (PMR) is a syndrome experienced as pain or stiffness, usually in the neck, shoulders, upper arms, and hips, but which may occur all over the body. The pain can be sudden or can occur gradually over a period. Most people with PMR wake up in the morning with pain in their muscles; however, cases have occurred in which the person has developed the pain during the evenings or has pain and stiffness all day long.

Podosomes are conical, actin-rich structures found on the outer surface of the plasma membrane of animal cells. Their size ranges from approximately 0.5 μm to 2.0 μm in diameter. While usually situated on the periphery of the cellular membrane, these unique structures display a polarized pattern of distribution in migrating cells, situating at the front border between the lamellipodium and lamellum. Their primary purpose is connected to cellular motility and invasion; therefore, they serve as both sites of attachment and degradation along the extracellular matrix. Many different specialized cells exhibit these dynamic structures such as invasive cancer cells, osteoclasts, vascular smooth muscle cells, endothelial cells, and certain immune cells like macrophages and dendritic cells.

Giant-cell tumor of the bone (GCTOB), is a relatively uncommon tumor of the bone. It is characterized by the presence of multinucleated giant cells. Malignancy in giant-cell tumor is uncommon and occurs in about 2% of all cases. However, if malignant degeneration does occur, it is likely to metastasize to the lungs. Giant-cell tumors are normally benign, with unpredictable behavior. It is a heterogeneous tumor composed of three different cell populations. The giant-cell tumour stromal cells (GCTSC) constitute the neoplastic cells, which are from an osteoblastic origin and are classified based on expression of osteoblast cell markers such as alkaline phosphatase and osteocalcin. In contrast, the mononuclear histiocytic cells (MNHC) and multinucleated giant cell (MNGC) fractions are secondarily recruited and comprise the non-neoplastic cell population. They are derived from an osteoclast-monocyte lineage determined primarily by expression of CD68, a marker for monocytic precursor cells. In most patients, the tumors are slow to develop, but may recur locally in as many as 50% of cases.

The chemokine ligand 2 (CCL2) is also referred to as monocyte chemoattractant protein 1 (MCP1) and small inducible cytokine A2. CCL2 is a small cytokine that belongs to the CC chemokine family. CCL2 tightly regulates cellular mechanics and thereby recruits monocytes, memory T cells, and dendritic cells to the sites of inflammation produced by either tissue injury or infection.

A histiocytoma in the dog is a benign tumor. It is an abnormal growth in the skin of histiocytes (histiocytosis), a cell that is part of the immune system. A similar disease in humans, Hashimoto-Pritzker disease, is also a Langerhans cell histiocytosis. Dog breeds that may be more at risk for this tumor include Bulldogs, American Pit Bull Terriers, American Staffordshire Terriers, Scottish Terriers, Greyhounds, Boxers, and Boston Terriers. They also rarely occur in goats and cattle.

Langhans giant cells (LGC) are giant cells found in granulomatous conditions.

CD68 is a protein highly expressed by cells in the monocyte lineage, by circulating macrophages, and by tissue macrophages.

According to a common point of view epithelioid cells are derivatives of activated macrophages resembling epithelial cells.
A fusion mechanism is any mechanism by which cell fusion or virus–cell fusion takes place, as well as the machinery that facilitates these processes. Cell fusion is the formation of a hybrid cell from two separate cells. There are three major actions taken in both virus–cell fusion and cell–cell fusion: the dehydration of polar head groups, the promotion of a hemifusion stalk, and the opening and expansion of pores between fusing cells. Virus–cell fusions occur during infections of several viruses that are health concerns relevant today. Some of these include HIV, Ebola, and influenza. For example, HIV infects by fusing with the membranes of immune system cells. In order for HIV to fuse with a cell, it must be able to bind to the receptors CD4, CCR5, and CXCR4. Cell fusion also occurs in a multitude of mammalian cells including gametes and myoblasts.
Multinucleate cells are eukaryotic cells that have more than one nucleus, i.e., multiple nuclei share one common cytoplasm. Mitosis in multinucleate cells can occur either in a coordinated, synchronous manner where all nuclei divide simultaneously or asynchronously where individual nuclei divide independently in time and space. Certain organisms may have a multinuclear stage of their life cycle. For example, slime molds have a vegetative, multinucleate life stage called a plasmodium.
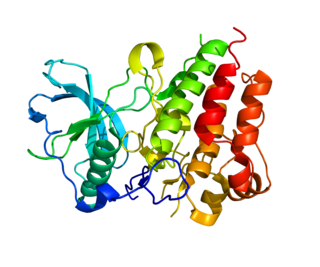
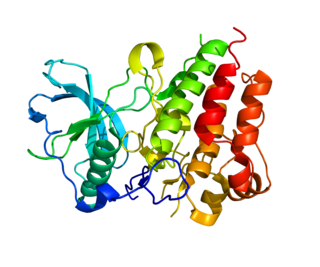
Colony stimulating factor 1 receptor (CSF1R), also known as macrophage colony-stimulating factor receptor (M-CSFR), and CD115, is a cell-surface protein encoded by the human CSF1R gene. CSF1R is a receptor that can be activated by two ligands: colony stimulating factor 1 (CSF-1) and interleukin-34 (IL-34). CSF1R is highly expressed in myeloid cells, and CSF1R signaling is necessary for the survival, proliferation, and differentiation of many myeloid cell types in vivo and in vitro. CSF1R signaling is involved in many diseases and is targeted in therapies for cancer, neurodegeneration, and inflammatory bone diseases.
Type IV hypersensitivity, in the Gell and Coombs classification of allergic reactions, often called delayed-type hypersensitivity, is a type of hypersensitivity reaction that can take a day or more to develop. Unlike the other types, it is not humoral but rather is a type of cell-mediated response. This response involves the interaction of T cells, monocytes, and macrophages.

A foreign-body giant cell is a collection of fused macrophages which are generated in response to the presence of a large foreign body. This is particularly evident with catheters, parasites, or biomaterials that are inserted into the body for replacement or regeneration of diseased or damaged tissues. Foreign body giant cells are also produced to digest foreign material that is too large for phagocytosis. The inflammatory process that creates these cells often leads to a foreign body granuloma.

Touton giant cells are a type of multinucleated giant cell seen in lesions with high lipid content such as fat necrosis, xanthoma, and xanthelasma and xanthogranulomas. They are also found in dermatofibroma.
Nikos Athanasou is a short story writer and novelist and musculoskeletal pathologist and scientist. He was born in Perth and grew up in Sydney where he studied medicine. He moved to England and is currently Professor of Musculoskeletal Pathology at Oxford University and a Fellow of Wadham College.