Related Research Articles

Haematopoiesis is the formation of blood cellular components. All cellular blood components are derived from haematopoietic stem cells. In a healthy adult human, roughly ten billion to a hundred billion new blood cells are produced per day, in order to maintain steady state levels in the peripheral circulation.
Agranulocytosis, also known as agranulosis or granulopenia, is an acute condition involving a severe and dangerous lowered white blood cell count and thus causing neutropenia in the circulating blood. It is a severe lack of one major class of infection-fighting white blood cells. People with this condition are at very high risk of serious infections due to their suppressed immune system.
Granulocytes are cells in the innate immune system characterized by the presence of specific granules in their cytoplasm. Such granules distinguish them from the various agranulocytes. All myeloblastic granulocytes are polymorphonuclear, that is, they have varying shapes (morphology) of the nucleus ; and are referred to as polymorphonuclear leukocytes. In common terms, polymorphonuclear granulocyte refers specifically to "neutrophil granulocytes", the most abundant of the granulocytes; the other types have varying morphology. Granulocytes are produced via granulopoiesis in the bone marrow.

Erythropoiesis is the process which produces red blood cells (erythrocytes), which is the development from erythropoietic stem cell to mature red blood cell.
A histiocyte is a vertebrate cell that is part of the mononuclear phagocyte system. The mononuclear phagocytic system is part of the organism's immune system. The histiocyte is a tissue macrophage or a dendritic cell. Part of their job is to clear out neutrophils once they've reached the end of their lifespan.

In immunology, agranulocytes are one of the two types of leukocytes, the other type being granulocytes. Agranular cells are noted by the absence of granules in their cytoplasm, which distinguishes them from granulocytes. Leukocytes are the first level of protection against disease. The two types of agranulocytes in the blood circulation are lymphocytes and monocytes. These make up about 35% of the hematologic blood values.

Granulocyte-macrophage colony-stimulating factor (GM-CSF), also known as colony-stimulating factor 2 (CSF2), is a monomeric glycoprotein secreted by macrophages, T cells, mast cells, natural killer cells, endothelial cells and fibroblasts that functions as a cytokine. The pharmaceutical analogs of naturally occurring GM-CSF are called sargramostim and molgramostim.

The myeloblast is a unipotent stem cell which differentiates into the effectors of the granulocyte series. It is found in the bone marrow. Stimulation of myeloblasts by G-CSF and other cytokines triggers maturation, differentiation, proliferation and cell survival.

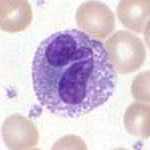
A myelocyte is a young cell of the granulocytic series, occurring normally in bone marrow.

Myeloid tissue, in the bone marrow sense of the word myeloid, is tissue of bone marrow, of bone marrow cell lineage, or resembling bone marrow, and myelogenous tissue is any tissue of, or arising from, bone marrow; in these senses the terms are usually used synonymously, as for example with chronic myeloid/myelogenous leukemia.
Hemopoietic growth factors regulate the differentiation and proliferation of particular progenitor cells. Made available through recombinant DNA technology, they hold tremendous potential for medical uses when a person's natural ability to form blood cells is diminished or defective. Recombinant erythropoietin (EPO) is very effective in treating the diminished red blood cell production that accompanies end-stage kidney disease. Erythropoietin is a sialoglycoprotein hormone produced by peritubular cells of kidney.

Monoblasts are the committed progenitor cells that differentiated from a committed macrophage or dendritic cell precursor (MDP) in the process of hematopoiesis. They are the first developmental stage in the monocyte series leading to a macrophage. Their myeloid cell fate is induced by the concentration of cytokines they are surrounded by during development. These cytokines induce the activation of transcription factors which push completion of the monoblast's myeloid cell fate. Monoblasts are normally found in bone marrow and do not appear in the normal peripheral blood. They mature into monocytes which, in turn, develop into macrophages. They then are seen as macrophages in the normal peripheral blood and many different tissues of the body. Macrophages can produce a variety of effector molecules that initiate local, systemic inflammatory responses. These monoblast differentiated cells are equipped to fight off foreign invaders using pattern recognition receptors to detect antigen as part of the innate immune response.

A promyelocyte is a granulocyte precursor, developing from the myeloblast and developing into the myelocyte. Promyelocytes measure 12-20 microns in diameter. The nucleus of a promyelocyte is approximately the same size as a myeloblast but their cytoplasm is much more abundant. They also have less prominent nucleoli than myeloblasts and their chromatin is more coarse and clumped. The cytoplasm is basophilic and contains primary red/purple granules.

Granulopoiesis is a part of haematopoiesis, that leads to the production of granulocytes. A granulocyte, also referred to as a polymorphonuclear leukocyte (PMN), is a type of white blood cell that has multi lobed nuclei, usually containing three lobes, and has a significant amount of cytoplasmic granules within the cell. Granulopoiesis takes place in the bone marrow. It leads to the production of three types of mature granulocytes: neutrophils, eosinophils and basophils.
CD16, also known as FcγRIII, is a cluster of differentiation molecule found on the surface of natural killer cells, neutrophils, monocytes, macrophages, and certain T cells. CD16 has been identified as Fc receptors FcγRIIIa (CD16a) and FcγRIIIb (CD16b), which participate in signal transduction. The most well-researched membrane receptor implicated in triggering lysis by NK cells, CD16 is a molecule of the immunoglobulin superfamily (IgSF) involved in antibody-dependent cellular cytotoxicity (ADCC). It can be used to isolate populations of specific immune cells through fluorescent-activated cell sorting (FACS) or magnetic-activated cell sorting, using antibodies directed towards CD16.
The following outline is provided as an overview of and topical guide to immunology:

CFU-GM, also known as granulocyte–macrophage progenitor (GMP), is a colony forming unit. It is derived from CFU-GEMM.

CFU-GEMM is a colony forming unit that generates myeloid cells. CFU-GEMM cells are the oligopotential progenitor cells for myeloid cells; they are thus also called common myeloid progenitor cells or myeloid stem cells. "GEMM" stands for granulocyte, erythrocyte, monocyte, megakaryocyte.

White blood cells, also called leukocytes or immune cells also called immunocytes, are cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. White blood cells include three main subtypes; granulocytes, lymphocytes and monocytes.

A white blood cell differential is a medical laboratory test that provides information about the types and amounts of white blood cells in a person's blood. The test, which is usually ordered as part of a complete blood count (CBC), measures the amounts of the five normal white blood cell types – neutrophils, lymphocytes, monocytes, eosinophils and basophils – as well as abnormal cell types if they are present. These results are reported as percentages and absolute values, and compared against reference ranges to determine whether the values are normal, low, or high. Changes in the amounts of white blood cells can aid in the diagnosis of many health conditions, including viral, bacterial, and parasitic infections and blood disorders such as leukemia.
References
- ↑ McGraw-Hill Concise Dictionary of Modern Medicine. S.v. "myelopoiesis." Retrieved 2022-03-15 from https://medical-dictionary.thefreedictionary.com/myelopoiesis
- ↑ Schultze, Joachim L.; Mass, Elvira; Schlitzer, Andreas (2019-02-19). "Emerging Principles in Myelopoiesis at Homeostasis and during Infection and Inflammation". Immunity. 50 (2): 288–301. doi: 10.1016/j.immuni.2019.01.019 . ISSN 1074-7613. PMID 30784577.
- ↑ Junqueira, Carneiro. Basic Histology, Text and Atlas.McGraw-Hill Companies. 2005. ISBN 978-0-07-144116-2