Red blood cells (RBCs), referred to as erythrocytes in academia and medical publishing, also known as red cells, erythroid cells, and rarely haematids, are the most common type of blood cell and the vertebrate's principal means of delivering oxygen to the body tissues—via blood flow through the circulatory system. Erythrocytes take up oxygen in the lungs, or in fish the gills, and release it into tissues while squeezing through the body's capillaries.

A myelodysplastic syndrome (MDS) is one of a group of cancers in which immature blood cells in the bone marrow do not mature, and as a result, do not develop into healthy blood cells. Early on, no symptoms typically are seen. Later, symptoms may include fatigue, shortness of breath, bleeding disorders, anemia, or frequent infections. Some types may develop into acute myeloid leukemia.
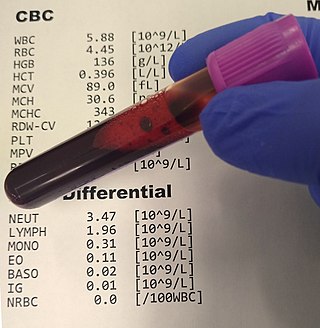
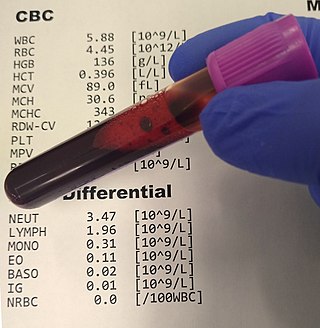
A complete blood count (CBC), also known as a full blood count (FBC), is a set of medical laboratory tests that provide information about the cells in a person's blood. The CBC indicates the counts of white blood cells, red blood cells and platelets, the concentration of hemoglobin, and the hematocrit. The red blood cell indices, which indicate the average size and hemoglobin content of red blood cells, are also reported, and a white blood cell differential, which counts the different types of white blood cells, may be included.

Fanconi anemia (FA) is a rare, autosomal recessive, genetic disease resulting in impaired response to DNA damage in the FA/BRCA pathway. Although it is a very rare disorder, study of this and other bone marrow failure syndromes has improved scientific understanding of the mechanisms of normal bone marrow function and development of cancer. Among those affected, the majority develop cancer, most often acute myelogenous leukemia (AML), MDS, and liver tumors. 90% develop aplastic anemia by age 40. About 60–75% have congenital defects, commonly short stature, abnormalities of the skin, arms, head, eyes, kidneys, and ears, and developmental disabilities. Around 75% have some form of endocrine problem, with varying degrees of severity. 60% of FA is FANC-A, 16q24.3, which has later onset bone marrow failure.

Hereditary spherocytosis (HS) is a congenital hemolytic disorder wherein a genetic mutation coding for a structural membrane protein phenotype causes the red blood cells to be sphere-shaped (spherocytosis), rather than the normal biconcave disk shape. This abnormal shape interferes with the cells' ability to flex during blood circulation, and also makes them more prone to rupture under osmotic stress, mechanical stress, or both. Cells with the dysfunctional proteins are degraded in the spleen, which leads to a shortage of erythrocytes and results in hemolytic anemia.

Erythropoiesis is the process which produces red blood cells (erythrocytes), which is the development from erythropoietic stem cell to mature red blood cell.

Pyruvate kinase deficiency is an inherited metabolic disorder of the enzyme pyruvate kinase which affects the survival of red blood cells. Both autosomal dominant and recessive inheritance have been observed with the disorder; classically, and more commonly, the inheritance is autosomal recessive. Pyruvate kinase deficiency is the second most common cause of enzyme-deficient hemolytic anemia, following G6PD deficiency.

Megaloblastic anemia is a type of macrocytic anemia. An anemia is a red blood cell defect that can lead to an undersupply of oxygen. Megaloblastic anemia results from inhibition of DNA synthesis during red blood cell production. When DNA synthesis is impaired, the cell cycle cannot progress from the G2 growth stage to the mitosis (M) stage. This leads to continuing cell growth without division, which presents as macrocytosis. Megaloblastic anemia has a rather slow onset, especially when compared to that of other anemias. The defect in red cell DNA synthesis is most often due to hypovitaminosis, specifically vitamin B12 deficiency or folate deficiency. Loss of micronutrients may also be a cause.

Reticulocytosis is a laboratory finding in which the number of reticulocytes in the bloodstream is elevated. Reticulocytes account for approximately 0.5% to 2.5% of the total red blood cells in healthy adults and 2% to 6% in infants, but in reticulocytosis, this percentage rises. Reticulocytes are produced in the bone marrow and then released into the bloodstream, where they mature into fully developed red blood cells between 1-2 days. Reticulocytosis often reflects the body’s response to conditions rather than an independent disease process and can arise from a variety of causes such as blood loss or anemia.

Left shift or blood shift is an increase in the number of immature cell types among the blood cells in a sample of blood. Many clinical mentions of left shift refer to the white blood cell lineage, particularly neutrophil-precursor band cells, thus signifying bandemia. Less commonly, left shift may also refer to a similar phenomenon in the red blood cell lineage in severe anemia, when increased reticulocytes and immature erythrocyte-precursor cells appear in the peripheral circulation.
Sideroblastic anemia, or sideroachrestic anemia, is a form of anemia in which the bone marrow produces ringed sideroblasts rather than healthy red blood cells (erythrocytes). In sideroblastic anemia, the body has iron available but cannot incorporate it into hemoglobin, which red blood cells need in order to transport oxygen efficiently. The disorder may be caused either by a genetic disorder or indirectly as part of myelodysplastic syndrome, which can develop into hematological malignancies.
The reticulocyte production index (RPI), also called a corrected reticulocyte count (CRC), is a calculated value used in the diagnosis of anemia. This calculation is necessary because the raw reticulocyte count is misleading in anemic patients. The problem arises because the reticulocyte count is not really a count but rather a percentage: it reports the number of reticulocytes as a percentage of the number of red blood cells. In anemia, the patient's red blood cells are depleted, creating an erroneously elevated reticulocyte count.
Reticulocytopenia is the medical term for an abnormal decrease in circulating red blood cell precursors (reticulocytes) that can lead to anemia due to resulting low red blood cell (erythrocyte) production. Reticulocytopenia may be an isolated finding or it may not be associated with abnormalities in other hematopoietic cell lineages such as those that produce white blood cells (leukocytes) or platelets (thrombocytes), a decrease in all three of these lineages is referred to as pancytopenia.
The term macrocytic is from Greek words meaning "large cell". A macrocytic class of anemia is an anemia in which the red blood cells (erythrocytes) are larger than their normal volume. The normal erythrocyte volume in humans is about 80 to 100 femtoliters. In metric terms the size is given in equivalent cubic micrometers. The condition of having erythrocytes which are too large, is called macrocytosis. In contrast, in microcytic anemia, the erythrocytes are smaller than normal.
Red blood cell indices are blood tests that provide information about the hemoglobin content and size of red blood cells. Abnormal values indicate the presence of anemia and which type of anemia it is.

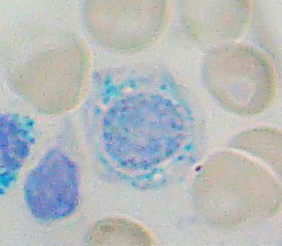
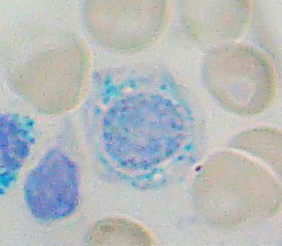
Pappenheimer bodies are abnormal basophilic granules of iron found inside red blood cells on routine blood stain. They are a type of inclusion body composed of ferritin aggregates, or mitochondria or phagosomes containing aggregated ferritin. They appear as dense, blue-purple granules within the red blood cell and there are usually only one or two, located in the cell periphery. They stain on a Romanowsky stain because clumps of ribosomes are co‐precipitated with the iron‐containing organelles.
Normocytic anemia is a type of anemia and is a common issue that occurs for men and women typically over 85 years old. Its prevalence increases with age, reaching 44 percent in men older than 85 years. The most common type of normocytic anemia is anemia of chronic disease.

Polychromasia is a disorder where there is an abnormally high number of immature red blood cells found in the bloodstream as a result of being prematurely released from the bone marrow during blood formation These cells are often shades of grayish-blue. Polychromasia is usually a sign of bone marrow stress as well as immature red blood cells. 3 types are recognized, with types 1 and 2 being referred to as 'young red blood cells' and type 3 as 'old red blood cells'. Giemsa stain is used to distinguish all three types of blood smears. The young cells will generally stain gray or blue in the cytoplasm. These young red blood cells are commonly called reticulocytes. All polychromatophilic cells are reticulocytes, however, not all reticulocytes are polychromatophilic. In the old blood cells, the cytoplasm either stains a light orange or does not stain at all.

A nucleated red blood cell (NRBC), also known by several other names, is a red blood cell that contains a cell nucleus. Almost all vertebrate organisms have hemoglobin-containing cells in their blood, and with the exception of mammals, all of these red blood cells are nucleated. In mammals, NRBCs occur in normal development as precursors to mature red blood cells in erythropoiesis, the process by which the body produces red blood cells.

A white blood cell differential is a medical laboratory test that provides information about the types and amounts of white blood cells in a person's blood. The test, which is usually ordered as part of a complete blood count (CBC), measures the amounts of the five normal white blood cell types – neutrophils, lymphocytes, monocytes, eosinophils and basophils – as well as abnormal cell types if they are present. These results are reported as percentages and absolute values, and compared against reference ranges to determine whether the values are normal, low, or high. Changes in the amounts of white blood cells can aid in the diagnosis of many health conditions, including viral, bacterial, and parasitic infections and blood disorders such as leukemia.