Red blood cells (RBCs), referred to as erythrocytes in academia and medical publishing, also known as red cells, erythroid cells, and rarely haematids, are the most common type of blood cell and the vertebrate's principal means of delivering oxygen to the body tissues—via blood flow through the circulatory system. Erythrocytes take up oxygen in the lungs, or in fish the gills, and release it into tissues while squeezing through the body's capillaries.

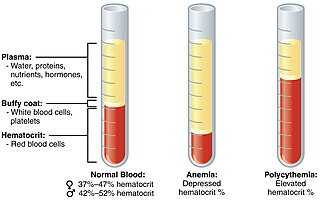
Anemia or anaemia is a blood disorder in which the blood has a reduced ability to carry oxygen. This can be due to a lower than normal number of red blood cells, a reduction in the amount of hemoglobin available for oxygen transport, or abnormalities in hemoglobin that impair its function.
Erythropoietin, also known as erythropoetin, haematopoietin, or haemopoietin, is a glycoprotein cytokine secreted mainly by the kidneys in response to cellular hypoxia; it stimulates red blood cell production (erythropoiesis) in the bone marrow. Low levels of EPO are constantly secreted in sufficient quantities to compensate for normal red blood cell turnover. Common causes of cellular hypoxia resulting in elevated levels of EPO include any anemia, and hypoxemia due to chronic lung disease and mouth disease.
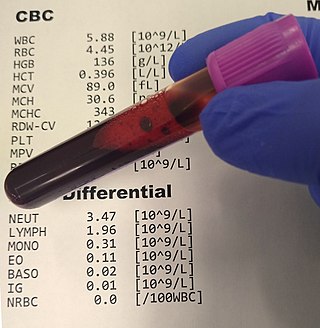
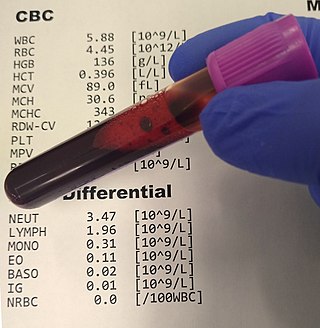
A complete blood count (CBC), also known as a full blood count (FBC), is a set of medical laboratory tests that provide information about the cells in a person's blood. The CBC indicates the counts of white blood cells, red blood cells and platelets, the concentration of hemoglobin, and the hematocrit. The red blood cell indices, which indicate the average size and hemoglobin content of red blood cells, are also reported, and a white blood cell differential, which counts the different types of white blood cells, may be included.

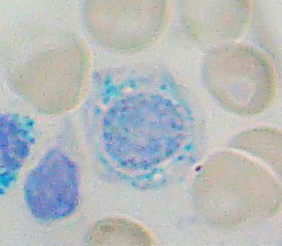
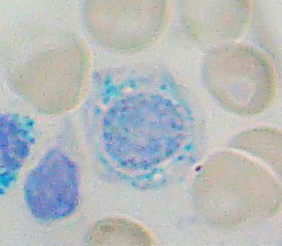
In hematology, reticulocytes are immature red blood cells (RBCs). In the process of erythropoiesis, reticulocytes develop and mature in the bone marrow and then circulate for about a day in the blood stream before developing into mature red blood cells. Like mature red blood cells, in mammals, reticulocytes do not have a cell nucleus. They are called reticulocytes because of a reticular (mesh-like) network of ribosomal RNA that becomes visible under a microscope with certain stains such as new methylene blue and Romanowsky stain.

The hematocrit, also known by several other names, is the volume percentage (vol%) of red blood cells (RBCs) in blood, measured as part of a blood test. The measurement depends on the number and size of red blood cells. It is normally 40.7–50.3% for males and 36.1–44.3% for females. It is a part of a person's complete blood count results, along with hemoglobin concentration, white blood cell count and platelet count.
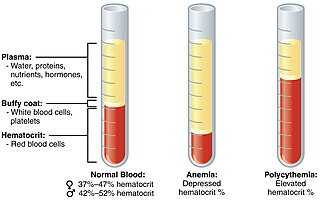
Polycythemia is a laboratory finding in which the hematocrit and/or hemoglobin concentration are increased in the blood. Polycythemia is sometimes called erythrocytosis, and there is significant overlap in the two findings, but the terms are not the same: polycythemia describes any increase in hematocrit and/or hemoglobin, while erythrocytosis describes an increase specifically in the number of red blood cells in the blood.
The mean corpuscular volume, or mean cell volume (MCV), is a measure of the average volume of a red blood corpuscle. The measure is obtained by multiplying a volume of blood by the proportion of blood that is cellular, and dividing that product by the number of erythrocytes in that volume. The mean corpuscular volume is a part of a standard complete blood count.

Erythropoiesis is the process which produces red blood cells (erythrocytes), which is the development from erythropoietic stem cell to mature red blood cell.

Hemolytic disease of the newborn, also known as hemolytic disease of the fetus and newborn, HDN, HDFN, or erythroblastosis fetalis, is an alloimmune condition that develops in a fetus at or around birth, when the IgG molecules produced by the mother pass through the placenta. Among these antibodies are some which attack antigens on the red blood cells in the fetal circulation, breaking down and destroying the cells. The fetus can develop reticulocytosis and anemia. The intensity of this fetal disease ranges from mild to very severe, and fetal death from heart failure can occur. When the disease is moderate or severe, many erythroblasts are present in the fetal blood, earning these forms of the disease the name erythroblastosis fetalis.

Reticulocytosis is a laboratory finding in which the number of reticulocytes in the bloodstream is elevated. Reticulocytes account for approximately 0.5% to 2.5% of the total red blood cells in healthy adults and 2% to 6% in infants, but in reticulocytosis, this percentage rises. Reticulocytes are produced in the bone marrow and then released into the bloodstream, where they mature into fully developed red blood cells between 1-2 days. Reticulocytosis often reflects the body’s response to conditions rather than an independent disease process and can arise from a variety of causes such as blood loss or anemia.
Anemia of chronic disease (ACD) or anemia of chronic inflammation is a form of anemia seen in chronic infection, chronic immune activation, and malignancy. These conditions all produce elevation of interleukin-6, which stimulates hepcidin production and release from the liver. Hepcidin production and release shuts down ferroportin, a protein that controls export of iron from the gut and from iron storing cells. As a consequence, circulating iron levels are reduced. Other mechanisms may also play a role, such as reduced erythropoiesis. It is also known as anemia of inflammation, or anemia of inflammatory response.
Sideroblastic anemia, or sideroachrestic anemia, is a form of anemia in which the bone marrow produces ringed sideroblasts rather than healthy red blood cells (erythrocytes). In sideroblastic anemia, the body has iron available but cannot incorporate it into hemoglobin, which red blood cells need in order to transport oxygen efficiently. The disorder may be caused either by a genetic disorder or indirectly as part of myelodysplastic syndrome, which can develop into hematological malignancies.
Reticulocytopenia is the medical term for an abnormal decrease in circulating red blood cell precursors (reticulocytes) that can lead to anemia due to resulting low red blood cell (erythrocyte) production. Reticulocytopenia may be an isolated finding or it may not be associated with abnormalities in other hematopoietic cell lineages such as those that produce white blood cells (leukocytes) or platelets (thrombocytes), a decrease in all three of these lineages is referred to as pancytopenia.
Anemia of prematurity (AOP) refers to a form of anemia affecting preterm infants with decreased hematocrit. AOP is a normochromic, normocytic hypoproliferative anemia. The primary mechanism of AOP is a decrease in erythropoietin (EPO), a red blood cell growth factor.
The term macrocytic is from Greek words meaning "large cell". A macrocytic class of anemia is an anemia in which the red blood cells (erythrocytes) are larger than their normal volume. The normal erythrocyte volume in humans is about 80 to 100 femtoliters. In metric terms the size is given in equivalent cubic micrometers. The condition of having erythrocytes which are too large, is called macrocytosis. In contrast, in microcytic anemia, the erythrocytes are smaller than normal.
Red blood cell indices are blood tests that provide information about the hemoglobin content and size of red blood cells. Abnormal values indicate the presence of anemia and which type of anemia it is.
Normocytic anemia is a type of anemia and is a common issue that occurs for men and women typically over 85 years old. Its prevalence increases with age, reaching 44 percent in men older than 85 years. The most common type of normocytic anemia is anemia of chronic disease.
Non-sideropenic hypochromic anemia also known as Normochromic Normocytic Anemia is a kind of anemia in which the red blood cells in circulation have a normal red color (normochromic) and the same size (normocytic). Normocytic normochromic anemia is most commonly caused by a variety of chronic infections and systemic diseases.

Polychromasia is a disorder where there is an abnormally high number of immature red blood cells found in the bloodstream as a result of being prematurely released from the bone marrow during blood formation These cells are often shades of grayish-blue. Polychromasia is usually a sign of bone marrow stress as well as immature red blood cells. 3 types are recognized, with types 1 and 2 being referred to as 'young red blood cells' and type 3 as 'old red blood cells'. Giemsa stain is used to distinguish all three types of blood smears. The young cells will generally stain gray or blue in the cytoplasm. These young red blood cells are commonly called reticulocytes. All polychromatophilic cells are reticulocytes, however, not all reticulocytes are polychromatophilic. In the old blood cells, the cytoplasm either stains a light orange or does not stain at all.