Low-molecular-weight heparin (LMWH) is a class of anticoagulant medications. They are used in the prevention of blood clots and, in the treatment of venous thromboembolism, and the treatment of myocardial infarction.

The partial thromboplastin time (PTT), also known as the activated partial thromboplastin time, is a blood test that characterizes coagulation of the blood. A historical name for this measure is the Kaolin-cephalin clotting time (KCCT), reflecting kaolin and cephalin as materials historically used in the test. Apart from detecting abnormalities in blood clotting, partial thromboplastin time is also used to monitor the treatment effect of heparin, a widely prescribed drug that reduces blood's tendency to clot.
Mixing studies are tests performed on blood plasma of patients or test subjects to distinguish factor deficiencies from factor inhibitors, such as lupus anticoagulant, or specific factor inhibitors, such as antibodies directed against factor VIII. Mixing studies are screening tests widely performed in coagulation laboratories. The basic purpose of these tests is to determine the cause of prolongation of Prothrombin Time (PT), Partial Thromboplastin Time, or sometimes of thrombin time (TT). Mixing studies take advantage of the fact that factor levels that are 50 percent of normal should give a normal Prothrombin time (PT) or Partial thromboplastin time (PTT) result.
Lupus anticoagulant is an immunoglobulin that binds to phospholipids and proteins associated with the cell membrane. Its name is a partial misnomer, as it is actually a prothrombotic antibody in vivo. The name derives from their properties in vitro, as these antibodies increase coagulation times in laboratory tests such as the activated partial thromboplastin time (aPTT). Investigators speculate that the antibodies interfere with phospholipids used to induce in vitro coagulation. In vivo, the antibodies are thought to interact with platelet membrane phospholipids, increasing adhesion and aggregation of platelets, which accounts for the in vivo prothrombotic characteristics.

Protein S deficiency is a disorder associated with increased risk of venous thrombosis. Protein S, a vitamin K-dependent physiological anticoagulant, acts as a nonenzymatic cofactor to activate protein C in the degradation of factor Va and factor VIIIa.

Hirudin is a naturally occurring peptide in the salivary glands of blood-sucking leeches that has a blood anticoagulant property. This is essential for the leeches' habit of feeding on blood, since it keeps a host's blood flowing after the worm's initial puncture of the skin.
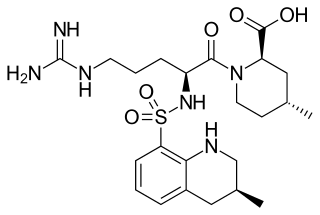
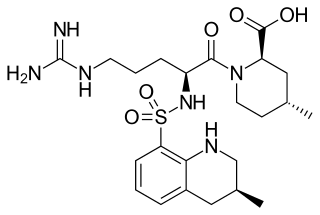
Argatroban is an anticoagulant that is a small molecule direct thrombin inhibitor. In 2000, argatroban was licensed by the US Food and Drug Administration (FDA) for prophylaxis or treatment of thrombosis in people with heparin-induced thrombocytopenia (HIT). In 2002, it was approved for use during percutaneous coronary interventions in people who have HIT or are at risk for developing it. In 2012, it was approved by the UK Medicines and Healthcare products Regulatory Agency for anticoagulation in people with heparin-induced thrombocytopenia Type II (HIT) who require parenteral antithrombotic therapy.
The prothrombinase enzyme complex consists of factor Xa (a serine protease) and factor Va (a protein cofactor). The complex assembles on negatively charged phospholipid membranes in the presence of calcium ions. The prothrombinase complex catalyzes the conversion of prothrombin (factor II), an inactive zymogen, to thrombin (factor IIa), an active serine protease. The activation of thrombin is a critical reaction in the coagulation cascade, which functions to regulate hemostasis in the body. To produce thrombin, the prothrombinase complex cleaves two peptide bonds in prothrombin, one after Arg271 and the other after Arg320. Although it has been shown that factor Xa can activate prothrombin when unassociated with the prothrombinase complex, the rate of thrombin formation is severely decreased under such circumstances. The prothrombinase complex can catalyze the activation of prothrombin at a rate 3 x 105-fold faster than can factor Xa alone. Thus, the prothrombinase complex is required for the efficient production of activated thrombin and also for adequate hemostasis.
Danaparoid sodium (Orgaran) is an anticoagulant with an antithrombotic action due to inhibition of thrombin generation (TGI) by two mechanisms: indirect inactivation of Factor Xa via AT and direct inhibition of thrombin activation of Factor IX. It also possesses a minor anti-thrombin activity, mediated equally via AT and Heparin Co-factor II producing a ratio of anti-Xa:IIa activity >22. [Meuleman DG. Haemostasis 1992;22:58-65 and Ofosu FA Haemostasis 1992;22:66-72]

The thrombin time (TT), also known as the thrombin clotting time (TCT), is a blood test that measures the time it takes for a clot to form in the plasma of a blood sample containing anticoagulant, after an excess of thrombin has been added. It is used to diagnose blood coagulation disorders and to assess the effectiveness of fibrinolytic therapy. This test is repeated with pooled plasma from normal patients. The difference in time between the test and the 'normal' indicates an abnormality in the conversion of fibrinogen to fibrin, an insoluble protein.
Direct thrombin inhibitors (DTIs) are a class of medication that act as anticoagulants by directly inhibiting the enzyme thrombin. Some are in clinical use, while others are undergoing clinical development. Several members of the class are expected to replace heparin and warfarin in various clinical scenarios.
Ecarin is an enzyme that is derived from the venom of the Indian saw-scaled viper, Echis carinatus, It is the primary reagent in the Ecarin clotting time test.
Hypercoagulability in pregnancy is the propensity of pregnant women to develop thrombosis. Pregnancy itself is a factor of hypercoagulability, as a physiologically adaptive mechanism to prevent post partum bleeding. However, when combined with an additional underlying hypercoagulable states, the risk of thrombosis or embolism may become substantial.
Direct factor Xa inhibitors (xabans) are anticoagulants, used to both treat and prevent blood clots in veins, and prevent stroke and embolism in people with atrial fibrillation (AF).
Thromboelastometry (TEM), previously named rotational thromboelastography (ROTEG) or rotational thromboelastometry (ROTEM), is an established viscoelastic method for hemostasis testing in whole blood. It is a modification of traditional thromboelastography (TEG).
Direct thrombin inhibitors (DTIs) are a class of anticoagulant drugs that can be used to prevent and treat embolisms and blood clots caused by various diseases. They inhibit thrombin, a serine protease which affects the coagulation cascade in many ways. DTIs have undergone rapid development since the 90's. With technological advances in genetic engineering the production of recombinant hirudin was made possible which opened the door to this new group of drugs. Before the use of DTIs the therapy and prophylaxis for anticoagulation had stayed the same for over 50 years with the use of heparin derivatives and warfarin which have some well known disadvantages. DTIs are still under development, but the research focus has shifted towards factor Xa inhibitors, or even dual thrombin and fXa inhibitors that have a broader mechanism of action by both inhibiting factor IIa (thrombin) and Xa. A recent review of patents and literature on thrombin inhibitors has demonstrated that the development of allosteric and multi-mechanism inhibitors might lead the way to a safer anticoagulant.
Thrombodynamics test is a method for blood coagulation monitoring and anticoagulant control. This test is based on imitation of coagulation processes occurring in vivo, is sensitive both to pro- and anticoagulant changes in the hemostatic balance. Highly sensitive to thrombosis.
Blood clotting tests are the tests used for diagnostics of the hemostasis system. Coagulometer is the medical laboratory analyzer used for testing of the hemostasis system. Modern coagulometers realize different methods of activation and observation of development of blood clots in blood or in blood plasma.
Prothrombin fragment 1+2 (F1+2), also written as prothrombin fragment 1.2 (F1.2), is a polypeptide fragment of prothrombin generated by the in vivo cleavage of prothrombin into thrombin by the enzyme prothrombinase. It is released from the N-terminus of prothrombin. F1+2 is a marker of thrombin generation and hence of coagulation activation. It is considered the best marker of in vivo thrombin generation.
The overall hemostatic potential (OHP) test is a global coagulation assay which can be used to measure coagulation. The OHP assay measures total fibrin generation in the presence of thrombin or tissue factor and tissue plasminogen activator (t-PA). It generates a fibrin time curve through the use of optical density measurement. This curve represents the balance between fibrin formation induced by thrombin or tissue factor and fibrinolysis induced by t-PA. The assay provides three parameters: overall coagulation potential (OCP), overall hemostatic potential (OHP), and overall fibrinolytic potential (OFP). OHP is the main parameter, while OCP and OFP are supplementary parameters to assess coagulation and fibrinolysis. One further parameter, clot lysis time (CLT), can also be determined. The OHP assay measures the integrated effect of procoagulant, anticoagulant, and fibrinolytic factors.