Related Research Articles

Platelets or thrombocytes are a component of blood whose function is to react to bleeding from blood vessel injury by clumping, thereby initiating a blood clot. Platelets have no cell nucleus; they are fragments of cytoplasm that are derived from the megakaryocytes of the bone marrow or lung, which then enter the circulation. Platelets are found only in mammals, whereas in other vertebrates, thrombocytes circulate as intact mononuclear cells.

Coagulation, also known as clotting, is the process by which blood changes from a liquid to a gel, forming a blood clot. It potentially results in hemostasis, the cessation of blood loss from a damaged vessel, followed by repair. The mechanism of coagulation involves activation, adhesion and aggregation of platelets, as well as deposition and maturation of fibrin.

Von Willebrand disease (VWD) is the most common hereditary blood-clotting disorder in humans. An acquired form can sometimes result from other medical conditions. It arises from a deficiency in the quality or quantity of von Willebrand factor (VWF), a multimeric protein that is required for platelet adhesion. It is known to affect several breeds of dogs as well as humans. The three forms of VWD are hereditary, acquired, and pseudo or platelet type. The three types of hereditary VWD are VWD type 1, VWD type 2, and VWD type 3. Type 2 contains various subtypes. Platelet type VWD is also an inherited condition.

Thrombotic thrombocytopenic purpura (TTP) is a blood disorder that results in blood clots forming in small blood vessels throughout the body. This results in a low platelet count, low red blood cells due to their breakdown, and often kidney, heart, and brain dysfunction. Symptoms may include large bruises, fever, weakness, shortness of breath, confusion, and headache. Repeated episodes may occur.
An assay is an investigative (analytic) procedure in laboratory medicine, mining, pharmacology, environmental biology and molecular biology for qualitatively assessing or quantitatively measuring the presence, amount, or functional activity of a target entity. The measured entity is often called the analyte, the measurand, or the target of the assay. The analyte can be a drug, biochemical substance, chemical element or compound, or cell in an organism or organic sample. An assay usually aims to measure an analyte's intensive property and express it in the relevant measurement unit.

(See also: List of proteins in the human body)

Glanzmann's thrombasthenia is an abnormality of the platelets. It is an extremely rare coagulopathy, in which the platelets contain defective or low levels of glycoprotein IIb/IIIa (GpIIb/IIIa), which is a receptor for fibrinogen. As a result, no fibrinogen bridging of platelets to other platelets can occur, and the bleeding time is significantly prolonged.

Bernard–Soulier syndrome (BSS) is a rare autosomal recessive bleeding disorder that is caused by a deficiency of the glycoprotein Ib-IX-V complex (GPIb-IX-V), the receptor for von Willebrand factor. The incidence of BSS is estimated to be less than 1 case per million persons, based on cases reported from Europe, North America, and Japan. BSS is a giant platelet disorder, meaning that it is characterized by abnormally large platelets.

Ristocetin is a glycopeptide antibiotic, obtained from Amycolatopsis lurida, previously used to treat staphylococcal infections. It is no longer used clinically because it caused thrombocytopenia and platelet agglutination. It is now used solely to assay those functions in vitro in the diagnosis of conditions such as von Willebrand disease (vWD) and Bernard–Soulier syndrome. Platelet agglutination caused by ristocetin can occur only in the presence of von Willebrand factor multimers, so if ristocetin is added to blood lacking the factor, the platelets will not clump.
Ripa or RIPA may refer to:
Glycoprotein Ib (GPIb), also known as CD42, is a component of the GPIb-V-IX complex on platelets. The GPIb-V-IX complex binds von Willebrand factor, allowing platelet adhesion and platelet plug formation at sites of vascular injury.
Platelet membrane glycoproteins are surface glycoproteins found on platelets (thrombocytes) which play a key role in hemostasis. When the blood vessel wall is damaged, platelet membrane glycoproteins interact with the extracellular matrix.

Platelet glycoprotein Ib alpha chain also known as glycoprotein Ib (platelet), alpha polypeptide or CD42b, is a protein that in humans is encoded by the GP1BA gene.

Glycoprotein Ib (platelet), beta polypeptide (GP1BB) also known as CD42c, is a protein that in humans is encoded by the GP1BB gene.

Glycoprotein IX (platelet) (GP9) also known as CD42a (Cluster of Differentiation 42a), is a human gene.
Cerastocytin is a thrombin-like serine protease in snake venom.

Giant platelet disorders, also known as macrothrombocytopenia, are rare disorders featuring abnormally large platelets, thrombocytopenia and a tendency to bleeding. Giant platelets cannot stick adequately to an injured blood vessel walls, resulting in abnormal bleeding when injured. Giant platelet disorder occurs for inherited diseases like Bernard–Soulier syndrome, gray platelet syndrome and May–Hegglin anomaly.
The GPIb-IX-V complex is a profuse membrane receptor complex originating in megakaryocytes and exclusively functional on the surface of platelets. It primarily functions to mediate the first critical step in platelet adhesion, by facilitating binding to von Willebrand factor (VWF) on damaged sub-endothelium under conditions of high fluid shear stress. Although the primary ligand for the GPIb-V-IX receptor is VWF, it can also bind to a number of other ligands in the circulation such as thrombin, P-selectin, factor XI, factor XII, high molecular weight kininogen as well as bacteria. GPIb-IX-V offers a critical role in thrombosis, metastasis, and the life cycle of platelets, and is implicated in a number of thrombotic pathological processes such as stroke or myocardial infarction.
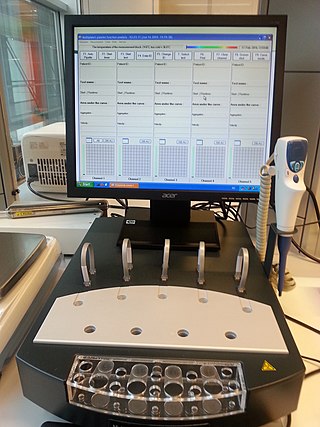
Multiplate multiple electrode aggregometry (MEA) is a test of platelet function in whole blood. The test can be used to diagnose platelet disorders, monitor antiplatelet therapy, and is also investigated as a potential predictor of transfusion requirements and bleeding risk in cardiac surgery.
The platelet plug, also known as the hemostatic plug or platelet thrombus, is an aggregation of platelets formed during early stages of hemostasis in response to one or more injuries to blood vessel walls. After platelets are recruited and begin to accumulate around the breakage, their “sticky” nature allows them to adhere to each other. This forms a platelet plug, which prevents more blood from leaving the body as well as any outside contaminants from getting in. The plug provides a temporary blockage of the break in the vasculature. As such, platelet plug formation occurs after vasoconstriction of the blood vessels but before the creation of the fibrin mesh clot, which is the more permanent solution to the injury. The result of the platelet plug formation is the coagulation of blood. It can also be referred to as primary hemostasis.
References
- ↑ Coller BS, Gralnick HR (August 1977). "Studies on the mechanism of ristocetin-induced platelet adhesion. Effects of structural modification of ristocetin and vancomycin". The Journal of Clinical Investigation. 60 (2): 302–12. doi:10.1172/JCI108778. PMC 372370 . PMID 17620.
- ↑ Riddell AF, Jenkins PV, Nitu-Whalley IC, McCraw AH, Lee CA, Brown, SA (January 2002). "Use of the collagen-binding assay for von Willebrand factor in the analysis of type 2M von Willebrand disease: a comparison with the ristocetin cofactor assay". British Journal of Haematology. 116 (1): 187–92. doi:10.1046/j.1365-2141.2002.03199.x. PMID 11841416. S2CID 40676013.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Pham A, Wang J. Bernard-Soulier syndrome: an inherited platelet disorder. Arch Pathol Lab Med (2007);131(12):1834-6.