Related Research Articles

A thrombus, colloquially called a blood clot, is the final product of the blood coagulation step in hemostasis. There are two components to a thrombus: aggregated platelets and red blood cells that form a plug, and a mesh of cross-linked fibrin protein. The substance making up a thrombus is sometimes called cruor. A thrombus is a healthy response to injury intended to stop and prevent further bleeding, but can be harmful in thrombosis, when a clot obstructs blood flow through healthy blood vessels in the circulatory system.

Coagulation, also known as clotting, is the process by which blood changes from a liquid to a gel, forming a blood clot. It potentially results in hemostasis, the cessation of blood loss from a damaged vessel, followed by repair. The mechanism of coagulation involves activation, adhesion and aggregation of platelets, as well as deposition and maturation of fibrin.

Disseminated intravascular coagulation (DIC) is a condition in which blood clots form throughout the body, blocking small blood vessels. Symptoms may include chest pain, shortness of breath, leg pain, problems speaking, or problems moving parts of the body. As clotting factors and platelets are used up, bleeding may occur. This may include blood in the urine, blood in the stool, or bleeding into the skin. Complications may include organ failure.

Fibrinogen is a glycoprotein complex, produced in the liver, that circulates in the blood of all vertebrates. During tissue and vascular injury, it is converted enzymatically by thrombin to fibrin and then to a fibrin-based blood clot. Fibrin clots function primarily to occlude blood vessels to stop bleeding. Fibrin also binds and reduces the activity of thrombin. This activity, sometimes referred to as antithrombin I, limits clotting. Fibrin also mediates blood platelet and endothelial cell spreading, tissue fibroblast proliferation, capillary tube formation, and angiogenesis and thereby promotes revascularization and wound healing.

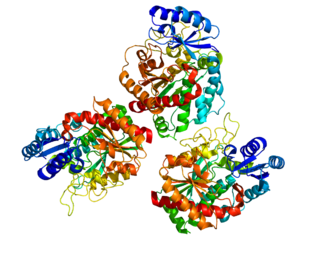
Thrombin is a serine protease, an enzyme that, in humans, is encoded by the F2 gene. During the clotting process, prothrombin is proteolytically cleaved by the prothrombinase enzyme complex to form thrombin. Thrombin in turn acts as a serine protease that converts soluble fibrinogen into insoluble strands of fibrin, as well as catalyzing many other coagulation-related reactions.
Fibrinolysis is a process that prevents blood clots from growing and becoming problematic. Primary fibrinolysis is a normal body process, while secondary fibrinolysis is the breakdown of clots due to a medicine, a medical disorder, or some other cause.
Thromboelastography (TEG) is a method of testing the efficiency of blood coagulation. It is a test mainly used in surgery and anesthesiology, although increasingly used in resuscitations in emergency departments, intensive care units, and labor and delivery suites. More common tests of blood coagulation include prothrombin time (PT) and partial thromboplastin time (aPTT) which measure coagulation factor function, but TEG also can assess platelet function, clot strength, and fibrinolysis which these other tests cannot.

The thrombin time (TT), also known as the thrombin clotting time (TCT), is a blood test that measures the time it takes for a clot to form in the plasma of a blood sample containing anticoagulant, after an excess of thrombin has been added. It is used to diagnose blood coagulation disorders and to assess the effectiveness of fibrinolytic therapy. This test is repeated with pooled plasma from normal patients. The difference in time between the test and the 'normal' indicates an abnormality in the conversion of fibrinogen to fibrin, an insoluble protein.
Carboxypeptidase B2 (CPB2), also known as carboxypeptidase U (CPU), plasma carboxypeptidase B (pCPB) or thrombin-activatable fibrinolysis inhibitor (TAFI), is an enzyme that, in humans, is encoded by the gene CPB2.
Thromboelastometry (TEM), previously named rotational thromboelastography (ROTEG) or rotational thromboelastometry (ROTEM), is an established viscoelastic method for hemostasis testing in whole blood. It is a modification of traditional thromboelastography (TEG).
Thrombodynamics test is a method for blood coagulation monitoring and anticoagulant control. This test is based on imitation of coagulation processes occurring in vivo, is sensitive both to pro- and anticoagulant changes in the hemostatic balance. Highly sensitive to thrombosis.
Blood clotting tests are the tests used for diagnostics of the hemostasis system. Coagulometer is the medical laboratory analyzer used for testing of the hemostasis system. Modern coagulometers realize different methods of activation and observation of development of blood clots in blood or in blood plasma.
The calibrated automated thrombogram is a thrombin generation assay (TGA) and global coagulation assay (GCA) which can be used as a coagulation test to assess thrombotic risk. It is the most widely used TGA. The CAT is a semi-automated test performed in a 96-well plate and requires specialized technologists to be performed. As a result, it has seen low implementation in routine laboratories and has been more limited to research settings. Lack of standardization with the CAT has also led to difficulties in study-to-study comparisons in research. However, efforts have recently been made towards standardization of the assay. An example of a specific commercial CAT is the Thrombinoscope by Thrombinoscope BV.
A thrombin generation assay (TGA) or thrombin generation test (TGT) is a global coagulation assay (GCA) and type of coagulation test which can be used to assess coagulation and thrombotic risk. It is based on the potential of a plasma to generate thrombin over time, following activation of coagulation via addition of phospholipids, tissue factor, and calcium. The results of the TGA can be output as a thrombogram or thrombin generation curve using computer software with calculation of thrombogram parameters.
The activated protein C resistance (APCR) test is a coagulation test used in the evaluation and diagnosis of activated protein C (APC) resistance, a form of hypercoagulability. Hereditary APC resistance is usually caused by the factor V Leiden mutation, whereas acquired APC resistance has been linked to antiphospholipid antibodies, pregnancy, and estrogen therapy. APC resistance can be measured using either an activated partial thromboplastin time (aPTT)-based test or an endogenous thrombin potential (ETP)-based test.
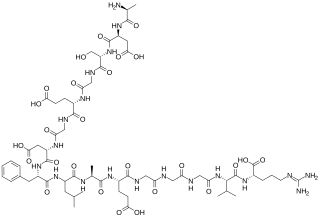
The fibrinopeptides, fibrinopeptide A (FpA) and fibrinopeptide B (FpB), are peptides which are located in the central region of the fibrous glycoprotein fibrinogen and are cleaved by the enzyme thrombin to convert fibrinogen into covalently-linked fibrin monomers. The N-terminal FpA is cleaved from the Aα chains of fibrinogen and FpB from the Bβ chains of fibrinogen, with FpA released before FpB. Subsequent to their formation, fibrin monomers are converted to cross-linked fibrin polymers by the action of thrombin-activated factor XIII, and these fibrin polymers form the backbone of a thrombus. Hence, the fibrinopeptides are sensitive markers of fibrinogenesis, thrombin activity, and coagulation.
Plasmin-α2-antiplasmin complex (PAP) is a 1:1 irreversibly formed inactive complex of the enzyme plasmin and its inhibitor α2-antiplasmin. It is a marker of the activity of the fibrinolytic system and a marker of net activation of fibrinolysis.
The ST Genesia is a fully automated commercial analyzer system for performing thrombin generation assays (TGAs) and hence for coagulation testing. It was developed by Diagnostica Stago and was introduced by the company in 2018.
Fibrin monomers are monomers of fibrin which are formed by the cleavage of fibrinogen by thrombin. Levels of fibrin monomers can be measured using blood tests and can serve as a marker of in vivo fibrinogenesis and coagulation activation. They may be useful in the evaluation hypercoagulability.
Coagulation activation markers are biomarkers of net activation of coagulation and fibrinolysis. Examples include prothrombin fragment 1+2 (F1+2), thrombin–antithrombin complex (TAT), fibrinopeptide A (FpA), fibrin monomers (FMs), plasmin-α2-antiplasmin complex (PAP), activated protein C–protein C inhibitor (APC-PCI), and D-dimer (DD). These compounds are markers of thrombin generation, fibrin generation, and fibrinolysis. Coagulation activation markers, particularly D-dimer, are useful in the diagnosis of acute venous thromboembolism. They may also be useful in the assessment of hypercoagulability and venous thromboembolism risk.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 Curnow J (2017). "The Overall Hemostatic Potential (OHP) Assay". Hemostasis and Thrombosis. Methods Mol Biol. Vol. 1646. pp. 523–531. doi:10.1007/978-1-4939-7196-1_38. ISBN 978-1-4939-7194-7. PMID 28804852.
- 1 2 3 4 5 6 Lim HY, Donnan G, Nandurkar H, Ho P (January 2022). "Global coagulation assays in hypercoagulable states". J Thromb Thrombolysis. 54 (1): 132–144. doi:10.1007/s11239-021-02621-1. PMID 34997471. S2CID 245804095.
- 1 2 3 4 5 6 7 8 9 10 Antovic A (October 2010). "The overall hemostasis potential: a laboratory tool for the investigation of global hemostasis". Semin Thromb Hemost. 36 (7): 772–9. doi:10.1055/s-0030-1265294. PMID 20978998. S2CID 35249276.
- 1 2 3 4 5 Antovic A (July 2008). "Screening haemostasis--looking for global assays: the Overall Haemostasis Potential (OHP) method--a possible tool for laboratory investigation of global haemostasis in both hypo- and hypercoagulable conditions". Curr Vasc Pharmacol. 6 (3): 173–85. doi:10.2174/157016108784912028. PMID 18673157.
- ↑ Lim HY, Leemaqz SY, Torkamani N, Grossmann M, Zajac JD, Nandurkar H, Ho P, Cheung AS (July 2020). "Global Coagulation Assays in Transgender Women on Oral and Transdermal Estradiol Therapy". J Clin Endocrinol Metab. 105 (7): e2369–e2377. doi: 10.1210/clinem/dgaa262 . PMID 32413907.
- ↑ He S, Bremme K, Blombäck M (October 1999). "A laboratory method for determination of overall haemostatic potential in plasma. I. Method design and preliminary results". Thromb Res. 96 (2): 145–56. doi:10.1016/s0049-3848(99)00092-4. PMID 10574592.
- ↑ He S, Antovic A, Blombäck M (September 2001). "A simple and rapid laboratory method for determination of haemostasis potential in plasma. II. Modifications for use in routine laboratories and research work". Thromb Res. 103 (5): 355–61. doi:10.1016/s0049-3848(01)00332-2. PMID 11553368.
- ↑ Curnow JL, Morel-Kopp MC, Roddie C, Aboud M, Ward CM (March 2007). "Reduced fibrinolysis and increased fibrin generation can be detected in hypercoagulable patients using the overall hemostatic potential assay". J Thromb Haemost. 5 (3): 528–34. doi:10.1111/j.1538-7836.2007.02362.x. PMID 17166248. S2CID 25346726.
- ↑ Curnow, J. L. (2010). Evaluation of the overall haemostatic potential assay for the diagnosis and management of hypercoagulable states (Doctoral dissertation, University of Sydney). https://scholar.google.com/scholar?cluster=17586055299192023070