Calculation
ANC =
or
ANC = (Absolute-Polys + Absolute-Bands)
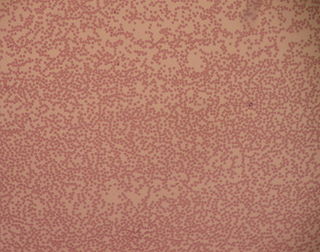
Absolute neutrophil count (ANC) is a measure of the number of neutrophil granulocytes [1] (also known as polymorphonuclear cells, PMN's, polys, granulocytes, segmented neutrophils or segs) present in the blood. Neutrophils are a type of white blood cell that fights against infection.
The ANC is almost always a part of a larger blood panel called the complete blood count. The ANC is calculated from measurements of the total number of white blood cells (WBC), usually based on the combined percentage of mature neutrophils (sometimes called "segs," or segmented cells) and bands, which are immature neutrophils.
The reference range for ANC in adults varies by study, but 1500 to 8000 cells per microliter is typical. An ANC less than 1500 cells/µL is defined as neutropenia and increases risk of infection. Neutropenia is the condition of a low ANC, and the most common condition where an ANC would be measured is in the setting of chemotherapy for cancer.[ citation needed ]
Neutrophilia indicates an elevated count. While many clinicians refer to the presence of neutrophilia as a "left shift," this is imprecise, as a left shift indicates the presence of immature neutrophil forms,[ citation needed ] but neutrophilia refers to the entire mass of neutrophils, both mature and immature. Neutrophilia can be indicative of:
ANC =
or
ANC = (Absolute-Polys + Absolute-Bands)
| Neutropenia Risk Category | ANC |
|---|---|
| Mild | ≥ 1000 to < 1500 cells/µL |
| Moderate | ≥ 500 to < 1000 cells/µL |
| Severe | < 500 cells/µL |
In some cases, a ratio is reported in addition to the sum. This is known as the "I/T ratio". [3] [4]
Agranulocytosis, also known as agranulosis or granulopenia, is an acute condition involving a severe and dangerous lowered white blood cell count and thus causing neutropenia in the circulating blood. It is a severe lack of one major class of infection-fighting white blood cells. People with this condition are at very high risk of serious infections due to their suppressed immune system.
Neutropenia is an abnormally low concentration of neutrophils in the blood. Neutrophils make up the majority of circulating white blood cells and serve as the primary defense against infections by destroying bacteria, bacterial fragments and immunoglobulin-bound viruses in the blood. People with neutropenia are more susceptible to bacterial infections and, without prompt medical attention, the condition may become life-threatening.

Neutrophilia is leukocytosis of neutrophils, that is, a high number of neutrophils in the blood. Because neutrophils are the main type of granulocytes, mentions of granulocytosis often overlap in meaning with neutrophilia.

Neutrophils are the most abundant type of granulocytes and make up 40% to 70% of all white blood cells in humans. They form an essential part of the innate immune system, with their functions varying in different animals.

Granulocyte colony-stimulating factor, also known as colony-stimulating factor 3, is a glycoprotein that stimulates the bone marrow to produce granulocytes and stem cells and release them into the bloodstream.
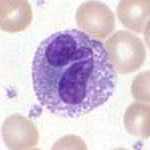
Granulocytes are cells in the innate immune system characterized by the presence of specific granules in their cytoplasm. Such granules distinguish them from the various agranulocytes. All myeloblastic granulocytes are polymorphonuclear. They have varying shapes (morphology) of the nucleus ; and are referred to as polymorphonuclear leukocytes. In common terms, polymorphonuclear granulocyte refers specifically to "neutrophil granulocytes", the most abundant of the granulocytes; the other types have varying morphology. Granulocytes are produced via granulopoiesis in the bone marrow.
In medicine, granulocytosis is the presence of an increased number of granulocytes in the peripheral blood. Often, the word refers to an increased neutrophil granulocyte count (neutrophilia), but granulocytosis formally refers to the combination of neutrophilia, eosinophilia, and basophilia. Leukocytosis refers to an increase in the number of all white blood cells.
Leukocytosis is a condition in which the white cell is above the normal range in the blood. It is frequently a sign of an inflammatory response, most commonly the result of infection, but may also occur following certain parasitic infections or bone tumors as well as leukemia. It may also occur after strenuous exercise, convulsions such as epilepsy, emotional stress, pregnancy and labor, anesthesia, as a side effect of medication, and epinephrine administration. There are five principal types of leukocytosis:

Leukopenia is a decrease in the number of leukocytes (WBC). Found in the blood, they are the white blood cells, and are the body's primary defense against an infection. Thus the condition of leukopenia places individuals at increased risk of infection.
The term leukemoid reaction describes an increased white blood cell count, which is a physiological response to stress or infection. It often describes the presence of immature cells such as myeloblasts or red blood cells with nuclei in the peripheral blood.
Cyclic neutropenia (CyN) is a rare hematologic disorder and form of congenital neutropenia that tends to occur approximately every three weeks and lasting for few days at a time due to changing rates of neutrophil production by the bone marrow. It causes a temporary condition with a low absolute neutrophil count and because the neutrophils make up the majority of circulating white blood cells it places the body at severe risk of inflammation and infection. In comparison to severe congenital neutropenia, it responds well to treatment with granulocyte colony-stimulating factor (filgrastim), which increases the neutrophil count, shortens the cycle length, as well decreases the severity and frequency of infections.
Severe congenital neutropenia (SCN), also often known as Kostmann syndrome or disease, is a group of rare disorders that affect myelopoiesis, causing a congenital form of neutropenia, usually without other physical malformations. SCN manifests in infancy with life-threatening bacterial infections. It causes severe pyogenic infections. It can be caused by autosomal dominant inheritance of the ELANE gene, autosomal recessive inheritance of the HAX1 gene. There is an increased risk of leukemia and Myelodysplastic cancers.

Left shift or blood shift is an increase in the number of immature cell types among the blood cells in a sample of blood. Many clinical mentions of left shift refer to the white blood cell lineage, particularly neutrophil-precursor band cells, thus signifying bandemia. Less commonly, left shift may also refer to a similar phenomenon in the red blood cell lineage in severe anemia, when increased reticulocytes and immature erythrocyte-precursor cells appear in the peripheral circulation.

Toxic granulation refers to dark coarse granules found in granulocytes, particularly neutrophils, in patients with inflammatory conditions.
Autoimmune neutropenia (AIN) is a form of neutropenia which is most common in infants and young children where the body identifies the neutrophils as enemies and makes antibodies to destroy them.
In hematology, myelopoiesis in the broadest sense of the term is the production of bone marrow and of all cells that arise from it, namely, all blood cells. In a narrower sense, myelopoiesis also refers specifically to the regulated formation of myeloid leukocytes (myelocytes), including eosinophilic granulocytes, basophilic granulocytes, neutrophilic granulocytes, and monocytes.

White blood cells, also called leukocytes or leucocytes, are cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. White blood cells include three main subtypes; granulocytes, lymphocytes and monocytes.

Toxic vacuolation, also known as toxic vacuolization, is the formation of vacuoles in the cytoplasm of neutrophils in response to severe infections or inflammatory conditions.

A white blood cell differential is a medical laboratory test that provides information about the types and amounts of white blood cells in a person's blood. The test, which is usually ordered as part of a complete blood count (CBC), measures the amounts of the five normal white blood cell types – neutrophils, lymphocytes, monocytes, eosinophils and basophils – as well as abnormal cell types if they are present. These results are reported as percentages and absolute values, and compared against reference ranges to determine whether the values are normal, low, or high. Changes in the amounts of white blood cells can aid in the diagnosis of many health conditions, including viral, bacterial, and parasitic infections and blood disorders such as leukemia.
A granulocyte transfusion is a medical procedure in which granulocytes are infused into a person's blood. Granulocyte transfusions were historically used to prevent and treat infections in people with neutropenia, but the practice declined in popularity in the 1980s. Interest in the procedure increased in the 1990s due to the development of more effective methods for harvesting granulocytes and a growing population of people with severe neutropenia from chemotherapy. However, the treatment's efficacy remains poorly understood and its use is controversial.