A myelodysplastic syndrome (MDS) is one of a group of cancers in which immature blood cells in the bone marrow do not mature, so do not become healthy blood cells. Early on, no symptoms typically are seen. Later, symptoms may include feeling tired, shortness of breath, bleeding disorders, anemia, or frequent infections. Some types may develop into acute myeloid leukemia.

Erythropoietin, also known as erythropoetin, haematopoietin, or haemopoietin, is a glycoprotein cytokine secreted mainly by the kidney in response to cellular hypoxia; it stimulates red blood cell production (erythropoiesis) in the bone marrow. Low levels of EPO are constantly secreted sufficient to compensate for normal red blood cell turnover. Common causes of cellular hypoxia resulting in elevated levels of EPO include any anemia, and hypoxemia due to chronic lung disease.

Erythropoiesis is the process which produces red blood cells (erythrocytes), which is the development from erythropoietic stem cell to mature red blood cell.

Plasma cells, also called plasma B cells, are white blood cells that originate in the bone marrow and secrete large quantities of proteins called antibodies in response to being presented specific substances called antigens. These antibodies are transported from the plasma cells by the blood plasma and the lymphatic system to the site of the target antigen, where they initiate its neutralization or destruction. B cells differentiate into plasma cells that produce antibody molecules closely modeled after the receptors of the precursor B cell.

The myeloblast is a unipotent stem cell which differentiates into the effectors of the granulocyte series. It is found in the bone marrow. Stimulation of myeloblasts by G-CSF and other cytokines triggers maturation, differentiation, proliferation and cell survival.
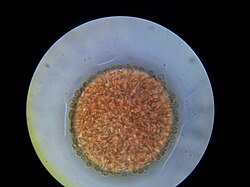
Sideroblastic anemia, or sideroachrestic anemia, is a form of anemia in which the bone marrow produces ringed sideroblasts rather than healthy red blood cells (erythrocytes). In sideroblastic anemia, the body has iron available but cannot incorporate it into hemoglobin, which red blood cells need in order to transport oxygen efficiently. The disorder may be caused either by a genetic disorder or indirectly as part of myelodysplastic syndrome, which can develop into hematological malignancies.
A myelocyte is a young cell of the granulocytic series, occurring normally in bone marrow.

Myeloid tissue, in the bone marrow sense of the word myeloid, is tissue of bone marrow, of bone marrow cell lineage, or resembling bone marrow, and myelogenous tissue is any tissue of, or arising from, bone marrow; in these senses the terms are usually used synonymously, as for example with chronic myeloid/myelogenous leukemia.

Acute erythroid leukemia is a rare form of acute myeloid leukemia where the myeloproliferation is of erythroblastic precursors. It is defined as type "M6" under the FAB classification.

GATA-binding factor 1 or GATA-1 is the founding member of the GATA family of transcription factors. This protein is widely expressed throughout vertebrate species. In humans and mice, it is encoded by the GATA1 and Gata1 genes, respectively. These genes are located on the X chromosome in both species.

The erythropoietin receptor (EpoR) is a protein that in humans is encoded by the EPOR gene. EpoR is a 52kDa peptide with a single carbohydrate chain resulting in an approximately 56-57 kDa protein found on the surface of EPO responding cells. It is a member of the cytokine receptor family. EpoR pre-exists as dimers which upon binding of a 30 kDa ligand erythropoietin (Epo), changes its homodimerized state. These conformational changes result in the autophosphorylation of Jak2 kinases that are pre-associated with the receptor. At present, the most well-established function of EpoR is to promote proliferation and rescue of erythroid progenitors from apoptosis.

Monoblasts are the committed progenitor cells that differentiated from myeloid stem cell in the process of hematopoiesis. They are normally found in bone marrow and do not appear in the normal peripheral blood. They mature into monocytes which, in turn, develop into macrophages.

A promyelocyte is a granulocyte precursor, developing from the myeloblast and developing into the myelocyte. Promyelocytes measure 12-20 microns in diameter. The nucleus of a promyelocyte is approximately the same size as a myeloblast but their cytoplasm is much more abundant. They also have less prominent nucleoli than myeloblasts and their chromatin is more coarse and clumped. The cytoplasm is basophilic and contains primary red/purple granules.

Granulopoiesis is a part of haematopoiesis, that leads to the production of granulocytes. A granulocyte, also referred to as polymorphonuclear lymphocyte (PMN), is a type of white blood cell that has multi lobed nuclei, usually containing three lobes, and has a significant amount of cytoplasmic granules within the cell. Granulopoiesis takes place in the bone marrow. It leads to the production of three types of mature granulocytes: neutrophils, eosinophils and basophils.
Lymphopoiesis (lĭm'fō-poi-ē'sĭs) is the generation of lymphocytes, one of the five types of white blood cell (WBC). It is more formally known as lymphoid hematopoiesis.

Homeobox protein Hox-A9 is a protein that in humans is encoded by the HOXA9 gene.
In hematology, myelopoiesis in the broadest sense of the term is the production of bone marrow and of all cells that arise from it, namely, all blood cells. In a narrower sense, myelopoiesis also refers specifically to the regulated formation of myeloid leukocytes (myelocytes), including eosinophilic granulocytes, basophilic granulocytes, neutrophilic granulocytes, and monocytes.

CFU-GEMM is a colony forming unit that generates myeloid cells. CFU-GEMM cells are the oligopotential progenitor cells for myeloid cells; they are thus also called common myeloid progenitor cells or myeloid stem cells. "GEMM" stands for granulocyte, erythrocyte, monocyte, megakaryocyte.

CFU-E stands for Colony Forming Unit-Erythroid. It arises from CFU-GEMM and gives rise to proerythroblasts.

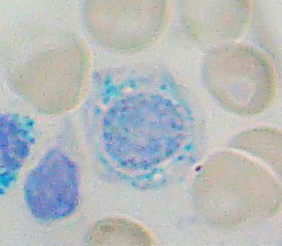
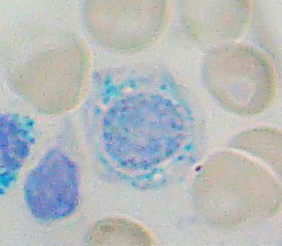
A nucleated red blood cell (NRBC), also known by several other names, is a red blood cell that contains a cell nucleus. Almost all vertebrate organisms have hemoglobin-containing cells in their blood, and with the exception of mammals, all of these red blood cells are nucleated. In mammals, NRBCs occur in normal development as precursors to mature red blood cells in erythropoiesis, the process by which the body produces red blood cells. NRBCs are normally found in the bone marrow of humans of all ages and in the blood of fetuses and newborn infants. After infancy, RBCs normally contain a nucleus only during the very early stages of the cell's life, and the nucleus is ejected as a normal part of cellular differentiation before the cell is released into the bloodstream. Thus, if NRBCs are identified on an adult's complete blood count or peripheral blood smear, it suggests that there is a very high demand for the bone marrow to produce RBCs, and immature RBCs are being released into circulation. Possible pathologic causes include anemia, myelofibrosis, thalassemia, miliary tuberculosis, cancers involving bone marrow, and in chronic hypoxemia.