Related Research Articles

Appendicitis is inflammation of the appendix. Symptoms commonly include right lower abdominal pain, nausea, vomiting, and decreased appetite. However, approximately 40% of people do not have these typical symptoms. Severe complications of a ruptured appendix include widespread, painful inflammation of the inner lining of the abdominal wall and sepsis.

Back pain is pain felt in the back. It may be classified as neck pain (cervical), middle back pain (thoracic), lower back pain (lumbar) or coccydynia based on the segment affected. The lumbar area is the most common area affected. An episode of back pain may be acute, subacute or chronic depending on the duration. The pain may be characterized as a dull ache, shooting or piercing pain or a burning sensation. Discomfort can radiate to the arms and hands as well as the legs or feet, and may include numbness or weakness in the legs and arms.

Constipation is a bowel dysfunction that makes bowel movements infrequent or hard to pass. The stool is often hard and dry. Other symptoms may include abdominal pain, bloating, and feeling as if one has not completely passed the bowel movement. Complications from constipation may include hemorrhoids, anal fissure or fecal impaction. The normal frequency of bowel movements in adults is between three per day and three per week. Babies often have three to four bowel movements per day while young children typically have two to three per day.

An emergency department (ED), also known as an accident and emergency department (A&E), emergency room (ER), emergency ward (EW) or casualty department, is a medical treatment facility specializing in emergency medicine, the acute care of patients who present without prior appointment; either by their own means or by that of an ambulance. The emergency department is usually found in a hospital or other primary care center.
Heartburn, also known as pyrosis, cardialgia or acid indigestion, is a burning sensation in the central chest or upper central abdomen. Heartburn is usually due to regurgitation of gastric acid into the esophagus. It is the major symptom of gastroesophageal reflux disease (GERD).

Bowel obstruction, also known as intestinal obstruction, is a mechanical or functional obstruction of the intestines which prevents the normal movement of the products of digestion. Either the small bowel or large bowel may be affected. Signs and symptoms include abdominal pain, vomiting, bloating and not passing gas. Mechanical obstruction is the cause of about 5 to 15% of cases of severe abdominal pain of sudden onset requiring admission to hospital.

Geriatrics, or geriatric medicine, is a medical specialty focused on providing care for the unique health needs of the elderly. The term geriatrics originates from the Greek γέρων geron meaning "old man", and ιατρός iatros meaning "healer". It aims to promote health by preventing, diagnosing and treating disease in older adults. There is no defined age at which patients may be under the care of a geriatrician, or geriatric physician, a physician who specializes in the care of older people. Rather, this decision is guided by individual patient need and the caregiving structures available to them. This care may benefit those who are managing multiple chronic conditions or experiencing significant age-related complications that threaten quality of daily life. Geriatric care may be indicated if caregiving responsibilities become increasingly stressful or medically complex for family and caregivers to manage independently.

Chest pain is pain or discomfort in the chest, typically the front of the chest. It may be described as sharp, dull, pressure, heaviness or squeezing. Associated symptoms may include pain in the shoulder, arm, upper abdomen, or jaw, along with nausea, sweating, or shortness of breath. It can be divided into heart-related and non-heart-related pain. Pain due to insufficient blood flow to the heart is also called angina pectoris. Those with diabetes or the elderly may have less clear symptoms.

Abdominal pain, also known as a stomach ache, is a symptom associated with both non-serious and serious medical issues. Since the abdomen contains most of the body's vital organs, it can be an indicator of a wide variety of diseases. Given that, approaching the examination of a person and planning of a differential diagnosis is extremely important.

In a physical examination, medical examination, clinical examination, or medical checkup, a medical practitioner examines a patient for any possible medical signs or symptoms of a medical condition. It generally consists of a series of questions about the patient's medical history followed by an examination based on the reported symptoms. Together, the medical history and the physical examination help to determine a diagnosis and devise the treatment plan. These data then become part of the medical record.
The medical history, case history, or anamnesis of a patient is a set of information the physicians collect over medical interviews. It involves the patient, and eventually people close to them, so to collect reliable/objective information for managing the medical diagnosis and proposing efficient medical treatments. The medically relevant complaints reported by the patient or others familiar with the patient are referred to as symptoms, in contrast with clinical signs, which are ascertained by direct examination on the part of medical personnel. Most health encounters will result in some form of history being taken. Medical histories vary in their depth and focus. For example, an ambulance paramedic would typically limit their history to important details, such as name, history of presenting complaint, allergies, etc. In contrast, a psychiatric history is frequently lengthy and in depth, as many details about the patient's life are relevant to formulating a management plan for a psychiatric illness.
The SOAP note is a method of documentation employed by healthcare providers to write out notes in a patient's chart, along with other common formats, such as the admission note. Documenting patient encounters in the medical record is an integral part of practice workflow starting with appointment scheduling, patient check-in and exam, documentation of notes, check-out, rescheduling, and medical billing. Additionally, it serves as a general cognitive framework for physicians to follow as they assess their patients.
Medically unexplained physical symptoms are symptoms for which a treating physician or other healthcare providers have found no medical cause, or whose cause remains contested. In its strictest sense, the term simply means that the cause for the symptoms is unknown or disputed—there is no scientific consensus. Not all medically unexplained symptoms are influenced by identifiable psychological factors. However, in practice, most physicians and authors who use the term consider that the symptoms most likely arise from psychological causes. Typically, the possibility that MUPS are caused by prescription drugs or other drugs is ignored. It is estimated that between 15% and 30% of all primary care consultations are for medically unexplained symptoms. A large Canadian community survey revealed that the most common medically unexplained symptoms are musculoskeletal pain, ear, nose, and throat symptoms, abdominal pain and gastrointestinal symptoms, fatigue, and dizziness. The term MUPS can also be used to refer to syndromes whose etiology remains contested, including chronic fatigue syndrome, fibromyalgia, multiple chemical sensitivity and Gulf War illness.

Emergency nursing is a specialty within the field of professional nursing focusing on the care of patients who require prompt medical attention to avoid long-term disability or death. In addition to addressing "true emergencies," emergency nurses increasingly care for people who are unwilling or unable to get primary medical care elsewhere and come to emergency departments for help. In fact, only a small percentage of emergency department (ED) patients have emergency conditions such as a stroke, heart attack or major trauma. Emergency nurses also tend to patients with acute alcohol and/or drug intoxication, psychiatric and behavioral problems and those who have been raped.
Emergency ultrasound employing point-of-care ultrasound (POCUS) is the application of ultrasound at the point of care to make immediate patient-care decisions. It is performed by the health care professional caring for the injured or ill persons. This point-of-care use of ultrasound is often to evaluate an emergency medical condition, in settings such as an emergency department, critical care unit, ambulance, or combat zone.
SOCRATES is a mnemonic acronym used by emergency medical services, physicians, nurses, and other health professionals to evaluate the nature of pain that a patient is experiencing.

Medical diagnosis is the process of determining which disease or condition explains a person's symptoms and signs. It is most often referred to as a diagnosis with the medical context being implicit. The information required for a diagnosis is typically collected from a history and physical examination of the person seeking medical care. Often, one or more diagnostic procedures, such as medical tests, are also done during the process. Sometimes the posthumous diagnosis is considered a kind of medical diagnosis.

Gender-biased diagnosing is the idea that medical and psychological diagnosis are influenced by the gender of the patient. Several studies have found evidence of differential diagnosis for patients with similar ailments but of different sexes. Female patients face discrimination through the denial of treatment or miss-classification of diagnosis as a result of not being taken seriously due to stereotypes and gender bias. According to traditional medical studies, most of these medical studies were done on men thus overlooking many issues that were related to women's health. This topic alone sparked controversy and brought about question to the medical standard of our time. Popular media has illuminated the issue of gender bias in recent years. Research that was done on diseases that affected women more were less funded than those diseases that affected men and women equally.
Undertreatment of pain is the absence of pain management therapy for a person in pain when treatment is indicated.
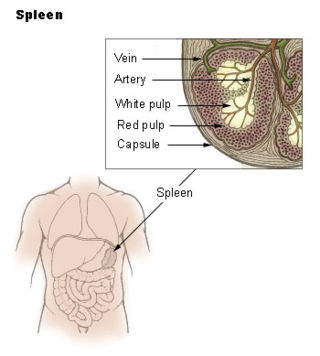
Spleen pain is a pain felt from the left upper quadrant of the abdomen or epigastrium where the human spleen is located or neighboring.
References
- ↑ Malmström T, Huuskonen O, Torkki P, Malmström R (November 2012). "Structured classification for ED presenting complaints - from free text field-based approach to ICPC-2 ED application". Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. 20 (1): 76. doi: 10.1186/1757-7241-20-76 . PMC 3564900 . PMID 23176447.
- ↑ "VI. Evaluation and Management (E/M) Services". Compliance Training Manual. www.usc.edu. Archived from the original on 2001-05-03.
- ↑ "coding q & a - Medical Vs. Vision Insurance". Optometric Management. July 1, 2004. Archived from the original on December 25, 2016.
- ↑ Shah N (2005). "Taking a history: Introduction and the presenting complaint". Student BMJ. 13: 309–52. doi:10.1136/sbmj.0509314. S2CID 155837706. Archived from the original on 2017-09-05.
- ↑ Bickley L (2017). Bates' Guide to Physical Examination and History Taking (12th ed.). Philadelphia: Wolters Kluwer. ISBN 9781469893419.
- ↑ "Implementation Guide for Transmission of Patient Chief Complaint as Public Health Information using Version 2.3.1 of the Health Level Seven (HL7) Standard Protocol" (PDF). Centers for Disease Control and Prevention. May 27, 2003. Archived from the original (PDF) on 2006-10-23.
- ↑ Nelson E, Kirk J, McHugo G, Douglass R, Ohler J, Wasson J, Zubkoff M (1987). "Chief complaint fatigue: a longitudinal study from the patient's perspective". Family Practice Research Journal. 6 (4): 175–88. PMID 3455125.
- ↑ Hussain N, Karnath B. "Differentiating Chest Pain". Emergency Medicine. Archived from the original on 2011-07-30.
- ↑ Graff LG, Robinson D (February 2001). "Abdominal pain and emergency department evaluation". Emergency Medicine Clinics of North America. 19 (1): 123–36. doi:10.1016/S0733-8627(05)70171-1. PMID 11214394.
- ↑ Ackermann RJ, Kemle KA, Vogel RL, Griffin RC (June 1998). "Emergency department use by nursing home residents". Annals of Emergency Medicine. 31 (6): 749–57. doi:10.1016/S0196-0644(98)70235-5. PMID 9624316.
- ↑ "Evaluation and Management Services Guide" (PDF). www.cms.gov. December 2010. Archived from the original (PDF) on 2012-04-11. Retrieved 2011-02-27.