Neuromyotonia (NMT) is a form of peripheral nerve hyperexcitability that causes spontaneous muscular activity resulting from repetitive motor unit action potentials of peripheral origin. NMT along with Morvan's syndrome are the most severe types in the Peripheral Nerve Hyperexciteability spectrum. Example of two more common and less severe syndromes in the spectrum are cramp fasciculation syndrome and benign fasciculation syndrome. NMT can have both hereditary and acquired (non-inherited) forms. The prevalence of NMT is unknown.

Neurology is the branch of medicine dealing with the diagnosis and treatment of all categories of conditions and disease involving the nervous system, which comprises the brain, the spinal cord and the peripheral nerves. Neurological practice relies heavily on the field of neuroscience, the scientific study of the nervous system.
Clinical neurophysiology is a medical specialty that studies the central and peripheral nervous systems through the recording of bioelectrical activity, whether spontaneous or stimulated. It encompasses both research regarding the pathophysiology along with clinical methods used to diagnose diseases involving both central and peripheral nervous systems. Examinations in the clinical neurophysiology field are not limited to tests conducted in a laboratory. It is thought of as an extension of a neurologic consultation. Tests that are conducted are concerned with measuring the electrical functions of the brain, spinal cord, and nerves in the limbs and muscles. It can give the precise definition of site, the type and degree of the lesion, along with revealing the abnormalities that are in question. Due to these abilities, clinical neurophysiology is used to mainly help diagnose diseases rather than treat them.
Morvan's syndrome is a rare, life-threatening autoimmune disease named after the nineteenth century French physician Augustin Marie Morvan. "La chorée fibrillaire" was first coined by Morvan in 1890 when describing patients with multiple, irregular contractions of the long muscles, cramping, weakness, pruritus, hyperhidrosis, insomnia and delirium. It normally presents with a slow insidious onset over months to years. Approximately 90% of cases spontaneously go into remission, while the other 10% of cases lead to death.
A demyelinating disease refers to any disease affecting the nervous system where the myelin sheath surrounding neurons is damaged. This damage disrupts the transmission of signals through the affected nerves, resulting in a decrease in their conduction ability. Consequently, this reduction in conduction can lead to deficiencies in sensation, movement, cognition, or other functions depending on the nerves affected.

Polyneuropathy is damage or disease affecting peripheral nerves in roughly the same areas on both sides of the body, featuring weakness, numbness, and burning pain. It usually begins in the hands and feet and may progress to the arms and legs and sometimes to other parts of the body where it may affect the autonomic nervous system. It may be acute or chronic. A number of different disorders may cause polyneuropathy, including diabetes and some types of Guillain–Barré syndrome.
Hypotonia is a state of low muscle tone, often involving reduced muscle strength. Hypotonia is not a specific medical disorder, but a potential manifestation of many different diseases and disorders that affect motor nerve control by the brain or muscle strength. Hypotonia is a lack of resistance to passive movement, whereas muscle weakness results in impaired active movement. Central hypotonia originates from the central nervous system, while peripheral hypotonia is related to problems within the spinal cord, peripheral nerves and/or skeletal muscles. Severe hypotonia in infancy is commonly known as floppy baby syndrome. Recognizing hypotonia, even in early infancy, is usually relatively straightforward, but diagnosing the underlying cause can be difficult and often unsuccessful. The long-term effects of hypotonia on a child's development and later life depend primarily on the severity of the muscle weakness and the nature of the cause. Some disorders have a specific treatment but the principal treatment for most hypotonia of idiopathic or neurologic cause is physical therapy and/or occupational therapy for remediation.

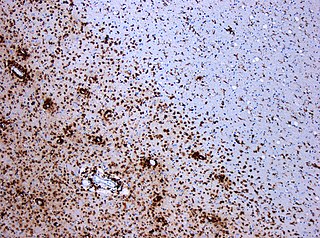
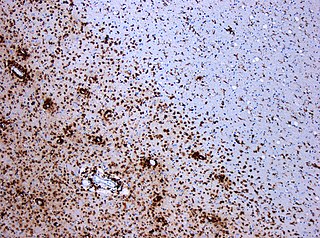
Neuropathology is the study of disease of nervous system tissue, usually in the form of either small surgical biopsies or whole-body autopsies. Neuropathologists usually work in a department of anatomic pathology, but work closely with the clinical disciplines of neurology, and neurosurgery, which often depend on neuropathology for a diagnosis. Neuropathology also relates to forensic pathology because brain disease or brain injury can be related to cause of death. Neuropathology should not be confused with neuropathy, which refers to disorders of the nerves themselves rather than the tissues. In neuropathology, the branches of the specializations of nervous system as well as the tissues come together into one field of study.

Neuritis, from the Greek νεῦρον), is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired transmission of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.

Foot drop is a gait abnormality in which the dropping of the forefoot happens out of weakness, irritation or damage to the deep fibular nerve, including the sciatic nerve, or paralysis of the muscles in the anterior portion of the lower leg. It is usually a symptom of a greater problem, not a disease in itself. Foot drop is characterized by inability or impaired ability to raise the toes or raise the foot from the ankle (dorsiflexion). Foot drop may be temporary or permanent, depending on the extent of muscle weakness or paralysis and it can occur in one or both feet. In walking, the raised leg is slightly bent at the knee to prevent the foot from dragging along the ground.

Gray matter heterotopia is a neurological disorder caused by gray matter being located in an atypical location in the brain.
Chronic inflammatory demyelinating polyneuropathy (CIDP) is an acquired autoimmune disease of the peripheral nervous system characterized by progressive weakness and impaired sensory function in the legs and arms. The disorder is sometimes called chronic relapsing polyneuropathy (CRP) or chronic inflammatory demyelinating polyradiculoneuropathy. CIDP is closely related to Guillain–Barré syndrome and it is considered the chronic counterpart of that acute disease. Its symptoms are also similar to progressive inflammatory neuropathy. It is one of several types of neuropathy.
Dysesthesia is an unpleasant, abnormal sense of touch. Its etymology comes from the Greek word "dys," meaning "bad," and "aesthesis," which means "sensation". It often presents as pain but may also present as an inappropriate, but not discomforting, sensation. It is caused by lesions of the nervous system, peripheral or central, and it involves sensations, whether spontaneous or evoked, such as burning, wetness, itching, electric shock, and pins and needles. Dysesthesia can include sensations in any bodily tissue, including most often the mouth, scalp, skin, or legs.
A paraneoplastic syndrome is a syndrome that is the consequence of a tumor in the body. It is specifically due to the production of chemical signaling molecules by tumor cells or by an immune response against the tumor. Unlike a mass effect, it is not due to the local presence of cancer cells.

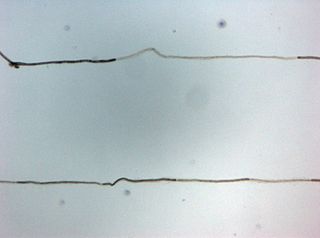
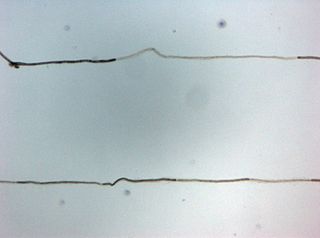
Group C nerve fibers are one of three classes of nerve fiber in the central nervous system (CNS) and peripheral nervous system (PNS). The C group fibers are unmyelinated and have a small diameter and low conduction velocity, whereas Groups A and B are myelinated. Group C fibers include postganglionic fibers in the autonomic nervous system (ANS), and nerve fibers at the dorsal roots. These fibers carry sensory information.

Cortical deafness is a rare form of sensorineural hearing loss caused by damage to the primary auditory cortex. Cortical deafness is an auditory disorder where the patient is unable to hear sounds but has no apparent damage to the structures of the ear. It has been argued to be as the combination of auditory verbal agnosia and auditory agnosia. Patients with cortical deafness cannot hear any sounds, that is, they are not aware of sounds including non-speech, voices, and speech sounds. Although patients appear and feel completely deaf, they can still exhibit some reflex responses such as turning their head towards a loud sound.
Pallesthesia, or vibratory sensation, is the ability to perceive vibration. This sensation, often conducted through skin and bone, is usually generated by mechanoreceptors such as Pacinian corpuscles, Merkel disk receptors, and tactile corpuscles. All of these receptors stimulate an action potential in afferent nerves found in various layers of the skin and body. The afferent neuron travels to the spinal column and then to the brain where the information is processed. Damage to the peripheral nervous system or central nervous system can result in a decline or loss of pallesthesia.

Neurological disorders represent a complex array of medical conditions that fundamentally disrupt the functioning of the nervous system. These disorders affect the brain, spinal cord, and nerve networks, presenting unique diagnosis, treatment, and patient care challenges. At their core, they represent disruptions to the intricate communication systems within the nervous system, stemming from genetic predispositions, environmental factors, infections, structural abnormalities, or degenerative processes.

Bonnet–Dechaume–Blanc syndrome, also known as Wyburn-Mason syndrome, is a rare congenital disorder characterized by arteriovenous malformations of the brain, retina or facial nevi. The syndrome has a number of possible symptoms and can, more rarely, affect the skin, bones, kidneys, muscles, and gastrointestinal tract. When the syndrome affects the brain, people can experience severe headaches, seizures, acute stroke, meningism, and progressive neurological deficits due to acute or chronic ischaemia caused by arteriovenous shunting.
Somatosensory evoked potential is the electrical activity of the brain that results from the stimulation of touch. SEP tests measure that activity and are a useful, noninvasive means of assessing somatosensory system functioning. By combining SEP recordings at different levels of the somatosensory pathways, it is possible to assess the transmission of the afferent volley from the periphery up to the cortex. SEP components include a series of positive and negative deflections that can be elicited by virtually any sensory stimuli. For example, SEPs can be obtained in response to a brief mechanical impact on the fingertip or to air puffs. However, SEPs are most commonly elicited by bipolar transcutaneous electrical stimulation applied on the skin over the trajectory of peripheral nerves of the upper limb or lower limb, and then recorded from the scalp. In general, somatosensory stimuli evoke early cortical components, generated in the contralateral primary somatosensory cortex (S1), related to the processing of the physical stimulus attributes. About 100 ms after stimulus application, additional cortical regions are activated, such as the secondary somatosensory cortex (S2), and the posterior parietal and frontal cortices, marked by a parietal P100 and bilateral frontal N140. SEPs are routinely used in neurology today to confirm and localize sensory abnormalities, to identify silent lesions and to monitor changes during surgical procedures.