The red-eye effect in photography is the common appearance of red pupils in color photographs of the eyes of humans and several other animals. It occurs when using a photographic flash that is very close to the camera lens in ambient low light.

Ophthalmology is a clinical and surgical specialty within medicine that deals with the diagnosis and treatment of eye disorders. A former term is oculism.

In neuroanatomy, the optic nerve, also known as the second cranial nerve, cranial nerve II, or simply CN II, is a paired cranial nerve that transmits visual information from the retina to the brain. In humans, the optic nerve is derived from optic stalks during the seventh week of development and is composed of retinal ganglion cell axons and glial cells; it extends from the optic disc to the optic chiasma and continues as the optic tract to the lateral geniculate nucleus, pretectal nuclei, and superior colliculus.
Cycloplegia is paralysis of the ciliary muscle of the eye, resulting in a loss of accommodation. Because of the paralysis of the ciliary muscle, the curvature of the lens can no longer be adjusted to focus on nearby objects. This results in similar problems as those caused by presbyopia, in which the lens has lost elasticity and can also no longer focus on close-by objects. Cycloplegia with accompanying mydriasis is usually due to topical application of muscarinic antagonists such as atropine and cyclopentolate.

Scanning laser ophthalmoscopy (SLO) is a method of examination of the eye. It uses the technique of confocal laser scanning microscopy for diagnostic imaging of the retina or cornea of the human eye.

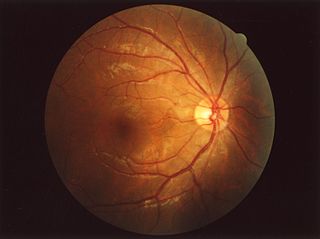
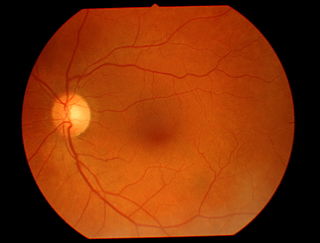
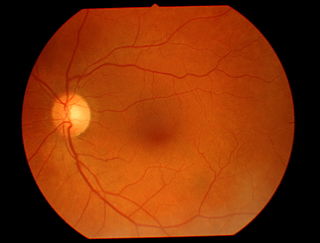
The optic disc or optic nerve head is the point of exit for ganglion cell axons leaving the eye. Because there are no rods or cones overlying the optic disc, it corresponds to a small blind spot in each eye.
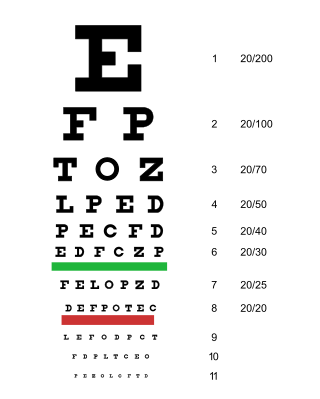
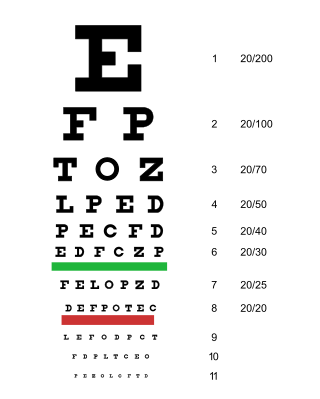
An eye examination is a series of tests performed to assess vision and ability to focus on and discern objects. It also includes other tests and examinations pertaining to the eyes. Eye examinations are primarily performed by an optometrist, ophthalmologist, or an orthoptist. Health care professionals often recommend that all people should have periodic and thorough eye examinations as part of routine primary care, especially since many eye diseases are asymptomatic.

In ophthalmology and optometry, a slit lamp is an instrument consisting of a high-intensity light source that can be focused to shine a thin sheet of light into the eye. It is used in conjunction with a biomicroscope. The lamp facilitates an examination of the anterior segment and posterior segment of the human eye, which includes the eyelid, sclera, conjunctiva, iris, natural crystalline lens, and cornea. The binocular slit-lamp examination provides a stereoscopic magnified view of the eye structures in detail, enabling anatomical diagnoses to be made for a variety of eye conditions. A second, hand-held lens is used to examine the retina.

Retinoscopy (Ret) is a technique to obtain an objective measurement of the refractive error of a patient's eyes. The examiner uses a retinoscope to shine light into the patient's eye and observes the reflection (reflex) off the patient's retina. While moving the streak or spot of light through the pupil across the retina, the examiner observes the relative movement of the reflex or manually places lenses over the eye to "neutralize" the reflex.

The posterior segment or posterior cavity is the back two-thirds of the eye that includes the anterior hyaloid membrane and all of the optical structures behind it: the vitreous humor, retina, choroid, and optic nerve. The portion of the posterior segment visible during ophthalmoscopy is sometimes referred to as the posterior pole, or fundus. Some ophthalmologists specialize in the treatment and management of posterior segment disorders and diseases.
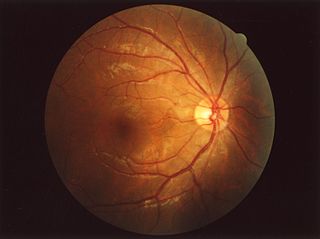
The fundus of the eye is the interior surface of the eye opposite the lens and includes the retina, optic disc, macula, fovea, and posterior pole. The fundus can be examined by ophthalmoscopy and/or fundus photography.

Dilated fundus examination (DFE) is a diagnostic procedure that uses mydriatic eye drops to dilate or enlarge the pupil in order to obtain a better view of the fundus of the eye. Once the pupil is dilated, examiners use ophthalmoscopy to view the eye's interior, which makes it easier to assess the retina, optic nerve head, blood vessels, and other important features. DFE has been found to be a more effective method for evaluating eye health when compared to non-dilated examination, and is the best method of evaluating structures behind the iris. It is frequently performed by ophthalmologists and optometrists as part of an eye examination.
The red reflex refers to the reddish-orange reflection of light from the back of the eye, or fundus, observed when using an ophthalmoscope or retinoscope. It is important to note that the red reflex may be absent or poorly visible in people with dark eyes, and may even appear yellow in Asians or green/blue in Africans.
Andreas Anagnostakis was a Greek ophthalmologist, physician, and educator. He is best known for inventing the ophthalmoscope, a handheld tool used in diagnostics and still relevant today. He is credited as the first ophthalmologist in Greece.

Fundus photography involves photographing the rear of an eye, also known as the fundus. Specialized fundus cameras consisting of an intricate microscope attached to a flash enabled camera are used in fundus photography. The main structures that can be visualized on a fundus photo are the central and peripheral retina, optic disc and macula. Fundus photography can be performed with colored filters, or with specialized dyes including fluorescein and indocyanine green.

Mammals normally have a pair of eyes. Although mammalian vision is not so excellent as bird vision, it is at least dichromatic for most of mammalian species, with certain families possessing a trichromatic color perception.
The eye is made up of the sclera, the iris, and the pupil, a black hole located at the center of the eye with the main function of allowing light to pass to the retina. Due to certain muscle spasms in the eye, the pupil can resemble a tadpole, which consists of a circular body, no arms or legs, and a tail.

The eagle eye is among the sharpest in the animal kingdom, with an eyesight estimated at 4 to 8 times stronger than that of the average human. Although an eagle may only weigh 10 pounds (4.5 kg), its eyes are roughly the same size as those of a human. Eagle weight varies: a small eagle could weigh 700 grams (1.5 lb), while a larger one could weigh 6.5 kilograms (14 lb); an eagle of about 10 kilograms (22 lb) weight could have eyes as big as that of a human who weighs 200 pounds (91 kg). Although the size of the eagle eye is about the same as that of a human being, the back side shape of the eagle eye is flatter. Their eyes are stated to be larger in size than their brain, by weight. Color vision with resolution and clarity are the most prominent features of eagles' eyes, hence sharp-sighted people are sometimes referred to as "eagle-eyed". Eagles can identify five distinctly colored squirrels and locate their prey even if hidden.
Teleophthalmology is a branch of telemedicine that delivers eye care through digital medical equipment and telecommunications technology. Today, applications of teleophthalmology encompass access to eye specialists for patients in remote areas, ophthalmic disease screening, diagnosis and monitoring; as well as distant learning.

The Heidelberg Retinal Tomography is a diagnostic procedure used in ophthalmology. The Heidelberg Retina Tomograph (HRT) is an ophthalmological confocal point scanning laser ophthalmoscope for examining the cornea and certain areas of the retina using different diagnostic modules. However, the most widely used area of application for HRT is the inspection of the optic nerve head (papilla) for early detection and follow-up of glaucoma. The procedure has established itself as an integral part of routine glaucoma diagnostics alongside the visual field examination (perimetry), the chamber angle examination (gonioscopy) and the measurement of intraocular pressure (tonometry). The HRT is the most widely used application of confocal scanning laser ophthalmoscopy.