Related Research Articles

Strabismus is a vision disorder in which the eyes do not properly align with each other when looking at an object. The eye that is pointed at an object can alternate. The condition may be present occasionally or constantly. If present during a large part of childhood, it may result in amblyopia, or lazy eyes, and loss of depth perception. If onset is during adulthood, it is more likely to result in double vision.

Eye surgery, also known as ophthalmic surgery or ocular surgery, is surgery performed on the eye or its adnexa. Eye surgery is part of ophthalmology and is performed by an ophthalmologist or eye surgeon. The eye is a fragile organ, and requires due care before, during, and after a surgical procedure to minimize or prevent further damage. An eye surgeon is responsible for selecting the appropriate surgical procedure for the patient, and for taking the necessary safety precautions. Mentions of eye surgery can be found in several ancient texts dating back as early as 1800 BC, with cataract treatment starting in the fifth century BC. It continues to be a widely practiced class of surgery, with various techniques having been developed for treating eye problems.

A chalazion or meibomian cyst is a cyst in the eyelid usually due to a blocked meibomian gland, typically in the middle of the eyelid, red, and not painful. They tend to come on gradually over a few weeks.

Minimally invasive procedures encompass surgical techniques that limit the size of incisions needed, thereby reducing wound healing time, associated pain, and risk of infection. Surgery by definition is invasive and many operations requiring incisions of some size are referred to as open surgery. Incisions made during open surgery can sometimes leave large wounds that may be painful and take a long time to heal. Advancements in medical technologies have enabled the development and regular use of minimally invasive procedures. For example, endovascular aneurysm repair, a minimally invasive surgery, has become the most common method of repairing abdominal aortic aneurysms in the US as of 2003. The procedure involves much smaller incisions than the corresponding open surgery procedure of open aortic surgery.

Duane syndrome is a congenital rare type of strabismus most commonly characterized by the inability of the eye to move outward. The syndrome was first described by ophthalmologists Jakob Stilling (1887) and Siegmund Türk (1896), and subsequently named after Alexander Duane, who discussed the disorder in more detail in 1905.
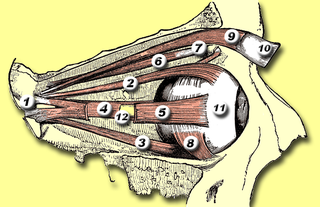
The inferior oblique muscle or obliquus oculi inferior is a thin, narrow muscle placed near the anterior margin of the floor of the orbit. The inferior oblique is one of the extraocular muscles, and is attached to the maxillary bone (origin) and the posterior, inferior, lateral surface of the eye (insertion). The inferior oblique is innervated by the inferior branch of the oculomotor nerve.

Blepharoplasty is the plastic surgery operation for correcting defects, deformities, and disfigurations of the eyelids; and for aesthetically modifying the eye region of the face. With the excision and the removal, or the repositioning of excess tissues, such as skin and adipocyte fat, and the reinforcement of the corresponding muscle and tendon tissues, the blepharoplasty procedure resolves functional and cosmetic problems of the periorbita, which is the area from the eyebrow to the upper portion of the cheek. The procedure is more common among women, who accounted for approximately 85% of blepharoplasty procedures in 2014 in the US and 88% of such procedures in the UK.

Trabeculectomy is a surgical procedure used in the treatment of glaucoma to relieve intraocular pressure by removing part of the eye's trabecular meshwork and adjacent structures. It is the most common glaucoma surgery performed and allows drainage of aqueous humor from within the eye to underneath the conjunctiva where it is absorbed. This outpatient procedure was most commonly performed under monitored anesthesia care using a retrobulbar block or peribulbar block or a combination of topical and subtenon anesthesia. Due to the higher risks associated with bulbar blocks, topical analgesia with mild sedation is becoming more common. Rarely general anesthesia will be used, in patients with an inability to cooperate during surgery.

Tenon's capsule, also known as the Tenon capsule, fascial sheath of the eyeball or the fascia bulbi, is a thin membrane which envelops the eyeball from the optic nerve to the corneal limbus, separating it from the orbital fat and forming a socket in which it moves.

Strabismus surgery is surgery on the extraocular muscles to correct strabismus, the misalignment of the eyes. Strabismus surgery is a one-day procedure that is usually performed under general anesthesia most commonly by either a neuro- or pediatric ophthalmologist. The patient spends only a few hours in the hospital with minimal preoperative preparation. After surgery, the patient should expect soreness and redness but is generally free to return home.
Polycoria is a pathological condition of the eye characterized by more than one pupillary opening in the iris. It may be congenital or result from a disease affecting the iris. It results in decreased function of the iris and pupil, affecting the physical eye and visualization.

An ocular prosthesis, artificial eye or glass eye is a type of craniofacial prosthesis that replaces an absent natural eye following an enucleation, evisceration, or orbital exenteration. The prosthesis fits over an orbital implant and under the eyelids. Though often referred to as a glass eye, the ocular prosthesis roughly takes the shape of a convex shell and is made of medical grade plastic acrylic. A few ocular prostheses today are made of cryolite glass. A variant of the ocular prosthesis is a very thin hard shell known as a scleral shell which can be worn over a damaged or eviscerated eye. Makers of ocular prosthetics are known as ocularists. An ocular prosthesis does not provide vision; this would be a visual prosthesis. Someone with an ocular prosthesis is altogether blind on the affected side and has monocular vision.
ReLExSmall incision lenticule extraction (SMILE), second generation of ReLEx Femtosecond lenticule extraction (FLEx), is a form of laser based refractive eye surgery developed by Carl Zeiss Meditec used to correct myopia, and cure astigmatism. Although similar to LASIK laser surgery, the intrastromal procedure uses a single femtosecond laser referenced to the corneal surface to cleave a thin lenticule from the corneal stroma for manual extraction.
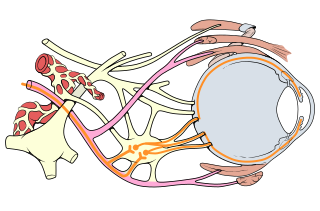
Oculomotor nerve palsy or oculomotor neuropathy is an eye condition resulting from damage to the third cranial nerve or a branch thereof. As the name suggests, the oculomotor nerve supplies the majority of the muscles controlling eye movements. Damage to this nerve will result in an inability to move the eye normally. The nerve also supplies the upper eyelid muscle and is accompanied by parasympathetic fibers innervating the muscles responsible for pupil constriction. The limitations of eye movement resulting from the condition are generally so severe that patients are often unable to maintain normal eye alignment when gazing straight ahead, leading to strabismus and, as a consequence, double vision (diplopia).

A laminotomy is an orthopaedic neurosurgical procedure that removes part of the lamina of a vertebral arch in order to relieve pressure in the vertebral canal. A laminotomy is less invasive than conventional vertebral column surgery techniques, such as laminectomy because it leaves more ligaments and muscles attached to the spinous process intact and it requires removing less bone from the vertebra. As a result, laminotomies typically have a faster recovery time and result in fewer postoperative complications. Nevertheless, possible risks can occur during or after the procedure like infection, hematomas, and dural tears. Laminotomies are commonly performed as treatment for lumbar spinal stenosis and herniated disks. MRI and CT scans are often used pre- and post surgery to determine if the procedure was successful.

Scleral reinforcement is a surgical procedure used to reduce or stop further macular damage caused by high myopia, which can be degenerative.
Botulinum toxin therapy of strabismus is a medical technique used sometimes in the management of strabismus, in which botulinum toxin is injected into selected extraocular muscles in order to reduce the misalignment of the eyes. The injection of the toxin to treat strabismus, reported upon in 1981, is considered to be the first ever use of botulinum toxin for therapeutic purposes. Today, the injection of botulinum toxin into the muscles that surround the eyes is one of the available options in the management of strabismus. Other options for strabismus management are vision therapy and occlusion therapy, corrective glasses and prism glasses, and strabismus surgery.
The management of strabismus may include the use of drugs or surgery to correct the strabismus. Agents used include paralytic agents such as botox used on extraocular muscles, topical autonomic nervous system agents to alter the refractive index in the eyes, and agents that act in the central nervous system to correct amblyopia.
Daniel Mojon is a Swiss ophthalmologist and ophthalmic surgeon who is considered to be the inventor of minimally invasive strabismus surgery (MISS), a method of surgically correcting squinting that uses only very small incisions of two to three millimeters and is supposed to lead to quicker rehabilitation and wound healing. Daniel Mojon is president of the program committee of the Swiss Academy of Ophthalmology (SAoO).
Manual small incision cataract surgery (MSICS) is an evolution of extracapsular cataract extraction (ECCE); the lens is removed from the eye through a self-sealing scleral tunnel wound. A well-constructed scleral tunnel is held closed by internal pressure, is watertight, and does not require suturing. The wound is relatively smaller than that in ECCE but is still markedly larger than a phacoemulsification wound. Comparative trials of MSICS against phaco in dense cataracts have found no difference in outcomes but MSICS had shorter operating times and significantly lower costs. MSICS has become the method of choice in the developing world because it provides high-quality outcomes with less surgically induced astigmatism than ECCE, no suture-related problems, quick rehabilitation, and fewer post-operative visits. MSICS is easy and fast to learn for the surgeon, cost effective, simple, and applicable to almost all types of cataract.
References
- ↑ D. S. Mojon: Comparison of a new, minimally invasive strabismus surgery technique with the usual limbal approach for rectus muscle recession and plication. In: Br J Ophthalmol. 91(1), Jan 2007, S. 76–82.
- ↑ M. H. Gobin, J. J. M. Bierlaagh: Chirurgie horizontale et cycloverticale simultane´e du strabisme. Centrum voor Strabologie, Antwerp 1994.
- ↑ D. S. Mojon: Review: minimally invasive strabismus surgery. In: Eye. 29, 2015, S. 225–233.
- ↑ Gupta P, Dadeya S, Kamlesh, Bhambhawani V: Comparison of Minimally Invasive Strabismus Surgery (MISS) and Conventional Strabismus Surgery Using the Limbal ApproachJ Pediatr Ophthalmol Strabismus. 2017;54:208-215.
- ↑ Kushner BJ. Minimally invasive strabismus surgery. Comparison of a new, minimally invasive strabismus surgery technique with the usual limbal approach for rectus muscle recession and plication. Br J Ophthalmol 2007;91:5.
- ↑ Asproudis I, Kozeis N, Katsanos A, Jain S, Tranos PG, Konstas AG. A Review of Minimally Invasive Strabismus Surgery (MISS): Is This the Way Forward?Adv Ther. 2017;34:826-833.
- ↑ D. S. Mojon: Review: minimally invasive strabismus surgery. In: Eye. 29, 2015, S. 225–233.
- ↑ P. Gupta, S. Dadeya, Kamlesh, V. Bhambhawani: Comparison of Minimally Invasive Strabismus Surgery (MISS) and Conventional Strabismus Surgery Using the Limbal Approach. In: J Pediatr Ophthalmol Strabismus. 54(4), 1. Jul 2017, S. 208–215.
- ↑ I. Asproudis, N. Kozeis, A. Katsanos, S. Jain, P. G. Tranos, A. G. Konstas: A Review of Minimally Invasive Strabismus Surgery (MISS): Is This the Way Forward? In: Adv Ther. 34(4), Apr 2017, S. 826–833.
- ↑ P. Merino, I. Blanco Domínguez, P. Gómez de Liaño: Outcomes of minimally invasive strabismus surgery for horizontal deviation. In: Arch Soc Esp Oftalmol. 91(2), Feb 2016, S. 69–73.
- ↑ N. Pellanda, D. S. Mojon: Combined horizontal rectus muscle minimally invasive strabismus surgery for exotropia. In: Can J Ophthalmol. 45(4), Aug 2010, S. 363–367.
- ↑ D. S. Mojon: Minimally invasive strabismus surgery for rectus muscle posterior fixation. In: Ophthalmologica. 223(2), 2009, S. 111–115.
- ↑ D. S. Mojon: Minimally invasive strabismus surgery (MISS) for inferior obliquus recession. In: Graefes Arch Clin Exp Ophthalmol. 247(2), 2009, S. 261–265.
- ↑ M. N. Naik, A. G. Nair, A. Gupta, S. Kamal: Minimally invasive surgery for thyroid eye disease. In: Indian J Ophthalmol. 63(11), Nov 2015, S. 847–853.
- ↑ D. S. Mojon: Review: minimally invasive strabismus surgery. In: Eye. 29, 2015, S. 225–233.