Steps
The exact procedures and techniques of the intravitreal injection varies among different guidelines, and may depend on the practices of the person performing the injection. Below is an example of the steps for the injection:
The patient usually leans back on the chair (in supine position), in which the headrest is stable and the patient is comfortable. [12] [34] Sterile drape is sometimes used to cover the face of the patient and only show the eye for the injection. [12] [36]
The specialist first applies anesthetics to the eye and eyelid to numb the area, so that the patient will not feel the pain during the procedure. [12] [22] [34] The type of anesthetic used depends on the practitioner practices and the patient's history. Some common forms of anesthetic used are eye drops (e.g. tetracaine/proparacaine) or gel (e.g. lidocaine 2% or 4% jelly), which is applied topically. [12] [34] Other choices of anesthesia include the use of lidocaine soaked pledget (a small cotton or wool pad) and subconjunctival injection (injection under the conjunctiva) of anesthetic agents. [23] However, the latter may cause a raised chance of subconjunctival hemorrhage. [12] Sometimes, for an eye with inflammation, a retrobulbar block may be given, but usually the topical or subconjunctival anesthesia is sufficient. [12] The anesthetic takes time to show the numbing effect, ranging from 1–5 minutes, depending on the chemical chosen. [12]
The specialist then sterilizes the eye and the surrounding area, often with povidone-iodine (PVP-I) solution, to prevent any infection in the injected site. [22] [34] Aqueous chlorhexidine is used instead in case of adverse effects to povidone-iodine. [23]
Next, an eyelid speculum is placed to retract the eyelids and thus hold the eye open. [22] [34] It helps to prevent contamination of the needle and the injection site by the eyelid or eyelashes. [37] Povidone-iodine solution is applied to the conjunctiva at the site of injection. [22] Another dose of local anesthetic may be given to the conjunctival surface again (for example, by placing a cotton swab soaked with the anesthetic drug solution over the targeted region), which is followed by the reapplication of PVP-I solution. [22]
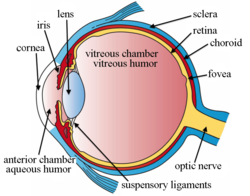
The injection site is measured and marked with a measuring caliper or other devices. [6] [36] The patient is then told to look away from the injection site to show the quadrant to be injected, and the doctor inserts the needle at the target site in a single motion into the mid-vitreous cavity. [12] Once the needle is in the vitreous cavity, the doctor pushes the plunger to release the drug into the cavity. [12] After that, the needle is removed, and the injection site is immediately covered with a cotton swab to avoid vitreous reflux (reflux of fluid from the vitreous cavity). [6] [12] The excess PVP-I solution is rinsed away. [12]
Finally, the doctor checks the patient's vision and intraocular pressure (IOP) of the eye. [12] The injection of certain medications, such as triamcinolone acetonide (Kenalog or Triesence), may cause a sudden increase in the IOP, [38] [39] and the patient should be monitored until the pressure returns to a normal level. If a large volume of drug is injected, paracentesis may be required. [12]