Related Research Articles

Hypoxia is a condition in which the body or a region of the body is deprived of adequate oxygen supply at the tissue level. Hypoxia may be classified as either generalized, affecting the whole body, or local, affecting a region of the body. Although hypoxia is often a pathological condition, variations in arterial oxygen concentrations can be part of the normal physiology, for example, during strenuous physical exercise.

The lungs are the main organs of the respiratory system in most terrestrial animals, including all tetrapod vertebrates and a small number of amphibious fish, pulmonate gastropods, and some arachnids. Their function is to conduct gas exchange by extracting oxygen from the air into the bloodstream via diffusion, and to release carbon dioxide from the bloodstream out into the atmosphere, a process also known as respiration. This article primarily concerns with the lungs of tetrapods, which are paired and located on either side of the heart, occupying most of the volume of the thoracic cavity, and are homologous to the swim bladders in ray-finned fish.

The respiratory system is a biological system consisting of specific organs and structures used for gas exchange in animals and plants. The anatomy and physiology that make this happen varies greatly, depending on the size of the organism, the environment in which it lives and its evolutionary history. In land animals, the respiratory surface is internalized as linings of the lungs. Gas exchange in the lungs occurs in millions of small air sacs; in mammals and reptiles, these are called alveoli, and in birds, they are known as atria. These microscopic air sacs have a very rich blood supply, thus bringing the air into close contact with the blood. These air sacs communicate with the external environment via a system of airways, or hollow tubes, of which the largest is the trachea, which branches in the middle of the chest into the two main bronchi. These enter the lungs where they branch into progressively narrower secondary and tertiary bronchi that branch into numerous smaller tubes, the bronchioles. In birds, the bronchioles are termed parabronchi. It is the bronchioles, or parabronchi that generally open into the microscopic alveoli in mammals and atria in birds. Air has to be pumped from the environment into the alveoli or atria by the process of breathing which involves the muscles of respiration.

A pulmonary alveolus, also known as an air sac or air space, is one of millions of hollow, distensible cup-shaped cavities in the lungs where pulmonary gas exchange takes place. Oxygen is exchanged for carbon dioxide at the blood–air barrier between the alveolar air and the pulmonary capillary. Alveoli make up the functional tissue of the mammalian lungs known as the lung parenchyma, which takes up 90 percent of the total lung volume.
Diffusing capacity of the lung (DL) measures the transfer of gas from air in the lung, to the red blood cells in lung blood vessels. It is part of a comprehensive series of pulmonary function tests to determine the overall ability of the lung to transport gas into and out of the blood. DL, especially DLCO, is reduced in certain diseases of the lung and heart. DLCO measurement has been standardized according to a position paper by a task force of the European Respiratory and American Thoracic Societies.

A bronchus is a passage or airway in the lower respiratory tract that conducts air into the lungs. The first or primary bronchi to branch from the trachea at the carina are the right main bronchus and the left main bronchus. These are the widest bronchi, and enter the right lung, and the left lung at each hilum. The main bronchi branch into narrower secondary bronchi or lobar bronchi, and these branch into narrower tertiary bronchi or segmental bronchi. Further divisions of the segmental bronchi are known as 4th order, 5th order, and 6th order segmental bronchi, or grouped together as subsegmental bronchi. The bronchi, when too narrow to be supported by cartilage, are known as bronchioles. No gas exchange takes place in the bronchi.

Gas exchange is the physical process by which gases move passively by diffusion across a surface. For example, this surface might be the air/water interface of a water body, the surface of a gas bubble in a liquid, a gas-permeable membrane, or a biological membrane that forms the boundary between an organism and its extracellular environment.

Asbestosis is long-term inflammation and scarring of the lungs due to asbestos fibers. Symptoms may include shortness of breath, cough, wheezing, and chest tightness. Complications may include lung cancer, mesothelioma, and pulmonary heart disease.

Spirometry is the most common of the pulmonary function tests (PFTs). It measures lung function, specifically the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. Spirometry is helpful in assessing breathing patterns that identify conditions such as asthma, pulmonary fibrosis, cystic fibrosis, and COPD. It is also helpful as part of a system of health surveillance, in which breathing patterns are measured over time.

Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD), is a group of respiratory diseases affecting the interstitium and space around the alveoli of the lungs. It concerns alveolar epithelium, pulmonary capillary endothelium, basement membrane, and perivascular and perilymphatic tissues. It may occur when an injury to the lungs triggers an abnormal healing response. Ordinarily, the body generates just the right amount of tissue to repair damage, but in interstitial lung disease, the repair process is disrupted, and the tissue around the air sacs (alveoli) becomes scarred and thickened. This makes it more difficult for oxygen to pass into the bloodstream. The disease presents itself with the following symptoms: shortness of breath, nonproductive coughing, fatigue, and weight loss, which tend to develop slowly, over several months. The average rate of survival for someone with this disease is between three and five years. The term ILD is used to distinguish these diseases from obstructive airways diseases.

Hypoxemia is an abnormally low level of oxygen in the blood. More specifically, it is oxygen deficiency in arterial blood. Hypoxemia has many causes, and often causes hypoxia as the blood is not supplying enough oxygen to the tissues of the body.
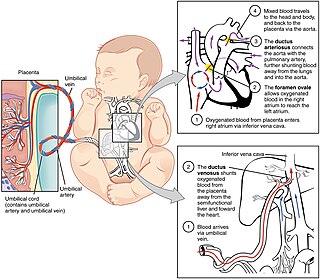
In humans, the circulatory system is different before and after birth. The fetal circulation is composed of the placenta, umbilical blood vessels encapsulated by the umbilical cord, heart and systemic blood vessels. A major difference between the fetal circulation and postnatal circulation is that the lungs are not used during the fetal stage resulting in the presence of shunts to move oxygenated blood and nutrients from the placenta to the fetal tissue. At birth, the start of breathing and the severance of the umbilical cord prompt various changes that quickly transform fetal circulation into postnatal circulation.
Positive end-expiratory pressure (PEEP) is the pressure in the lungs above atmospheric pressure that exists at the end of expiration. The two types of PEEP are extrinsic PEEP and intrinsic PEEP. Pressure that is applied or increased during an inspiration is termed pressure support. PEEP is a therapeutic parameter set in the ventilator, or a complication of mechanical ventilation with air trapping (auto-PEEP).
A pulmonary shunt is the passage of deoxygenated blood from the right side of the heart to the left without participation in gas exchange in the pulmonary capillaries. It is a pathological condition that results when the alveoli of parts of the lungs are perfused with blood as normal, but ventilation fails to supply the perfused region. In other words, the ventilation/perfusion ratio of those areas is zero.
The factors that determine the values for alveolar pO2 and pCO2 are:

Chloride shift (also known as the Hamburger phenomenon or lineas phenomenon, named after Hartog Jakob Hamburger) is a process which occurs in a cardiovascular system and refers to the exchange of bicarbonate (HCO3−) and chloride (Cl−) across the membrane of red blood cells (RBCs).

A pulmonary contusion, also known as lung contusion, is a bruise of the lung, caused by chest trauma. As a result of damage to capillaries, blood and other fluids accumulate in the lung tissue. The excess fluid interferes with gas exchange, potentially leading to inadequate oxygen levels (hypoxia). Unlike pulmonary laceration, another type of lung injury, pulmonary contusion does not involve a cut or tear of the lung tissue.
Indium lung is a rare occupational lung disease caused by exposure to respirable indium in the form of indium tin oxide. It is classified as an interstitial lung disease.
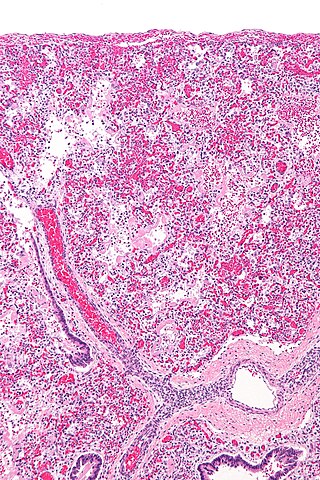
The pathophysiology of acute respiratory distress syndrome involves fluid accumulation in the lungs not explained by heart failure. It is typically provoked by an acute injury to the lungs that results in flooding of the lungs' microscopic air sacs responsible for the exchange of gases such as oxygen and carbon dioxide with capillaries in the lungs. Additional common findings in ARDS include partial collapse of the lungs (atelectasis) and low levels of oxygen in the blood (hypoxemia). The clinical syndrome is associated with pathological findings including pneumonia, eosinophilic pneumonia, cryptogenic organizing pneumonia, acute fibrinous organizing pneumonia, and diffuse alveolar damage (DAD). Of these, the pathology most commonly associated with ARDS is DAD, which is characterized by a diffuse inflammation of lung tissue. The triggering insult to the tissue usually results in an initial release of chemical signals and other inflammatory mediators secreted by local epithelial and endothelial cells.

Ventilation–perfusion coupling is the relationship between ventilation and perfusion processes, which take place in the respiratory system and the cardiovascular system. Ventilation is the movement of gas during breathing, and perfusion is the process of pulmonary blood circulation, which delivers oxygen to body tissues. Anatomically, the lung structure, alveolar organization, and alveolar capillaries contribute to the physiological mechanism of ventilation and perfusion. Ventilation–perfusion coupling maintains a constant ventilation/perfusion ratio near 0.8 on average, while the regional variation exists within the lungs due to gravity. When the ratio gets above or below 0.8, it is considered abnormal ventilation-perfusion coupling, also known as a ventilation–perfusion mismatch. Lung diseases, cardiac shunts, and smoking can cause a ventilation-perfusion mismatch that results in significant symptoms and diseases, which can be treated through treatments like bronchodilators and oxygen therapy.
References
- ↑ Macintyre N, Crapo RO, Viegi G, et al. (October 2005). "Standardisation of the single-breath determination of carbon monoxide uptake in the lung". Eur. Respir. J. 26 (4): 720–35. doi: 10.1183/09031936.05.00034905 . PMID 16204605.
- ↑ Hughes J, Bates D (2003). "Historical review: the carbon monoxide diffusing capacity (DLCO) and its membrane (DM) and red cell (Theta.Vc) components". Respir Physiol Neurobiol. 138 (2–3): 115–42. doi:10.1016/j.resp.2003.08.004. PMID 14609505. S2CID 35335150.
- ↑ Sue, DY; Oren, A; Hansen, JE; Wasserman, K (1987). "Diffusing capacity for carbon monoxide as a predictor of gas exchange during exercise". N. Engl. J. Med. 316 (21): 1301–1306. doi:10.1056/nejm198705213162103. PMID 3574401.
- ↑ American Thoracic society, Single Breath Carbon Monoxide Diffusing Capacity (transfer factor) Recommendations for a Standard Technique- 1995 Update, Am J Respir Crit Care Med. 152 pp 2185-2198 (1995).
- ↑ J.E. Cotes 1993, Lung Function, 5th Edition., Blackwell Scientific Publications, London
- ↑ J.E. Cotes, J.M. Dabbs, P.C. Elwood, A.M. Hall, A. McDonald, and M.J. Saunders. Iron-deficiency anaemia: its effects on transfer factor for the lung (diffusing capacity) and ventilation and cardiac frequency during submaximal exercise. Clin. Sci. 42:325-33 (1972).
- ↑ Bailey, Kristina L. (1 July 2012). "The Importance of the Assessment of Pulmonary Function in COPD". The Medical Clinics of North America. 96 (4): 745–752. doi:10.1016/j.mcna.2012.04.011. ISSN 0025-7125. PMC 3998207 . PMID 22793942.
- ↑ Puri, Sundeep (1 Jun 1995). "Reduced Alveolar–Capillary Membrane Diffusing Capacity in Chronic Heart Failure". Circulation. 91 (11): 2769–2774. doi:10.1161/01.CIR.91.11.2769. PMID 7758183.
- ↑ Ruppel, G. L. (2009). Manual of Pulmonary Function Testing. ISBN 978-0-323-05212-2
- ↑ "2017 ERS/ATS standards for single-breath carbon monoxide uptake in the lung" (PDF). European Respiratory Journal.
- ↑ Nguyen, Lam-Phuong; Harper, Richart W.; Louie, Samuel (2016). "Using and Interpreting Carbon Monoxide Diffusing Capacity (Dlco) Correctly". Consultant.
- ↑ Diffusion lung capacity for carbon monoxide (DLCO) is an independent prognostic factor for long-term survival after curative lung resection for cancer (p n/a) Michael J. Liptay, Sanjib Basu, Michael C. Hoaglin, Neil Freedman, L. Penfield Faber, William H. Warren, Zane T. Hammoud, Anthony W. Kim. Journal of Surgical Oncology. Published Online: Oct 1 2009 8:20AM doi : 10.1002/jso.21407