Transcranial magnetic stimulation (TMS) is a noninvasive form of brain stimulation in which a changing magnetic field is used to induce an electric current at a specific area of the brain through electromagnetic induction. An electric pulse generator, or stimulator, is connected to a magnetic coil connected to the scalp. The stimulator generates a changing electric current within the coil which creates a varying magnetic field, inducing a current within a region in the brain itself.
Tinnitus is a variety of sound that is heard when no corresponding external sound is present. Nearly everyone experiences faint "normal tinnitus" in a completely quiet room; but it is of concern only if it is bothersome, interferes with normal hearing, or is associated with other problems. The word tinnitus comes from the Latin tinnire, "to ring". In some people, it interferes with concentration, and can be associated with anxiety and depression.
Exploding head syndrome (EHS) is an abnormal sensory perception during sleep in which a person experiences auditory hallucinations that are loud and of short duration when falling asleep or waking up. The noise may be frightening, typically occurs only occasionally, and is not a serious health concern. People may also experience a flash of light. Pain is typically absent.
Visual snow syndrome (VSS) is an uncommon neurological condition in which the primary symptom is that affected individuals see persistent flickering white, black, transparent, or coloured dots across the whole visual field. Other common symptoms are palinopsia, enhanced entoptic phenomena, photophobia, and tension headaches. The condition is typically always present and has no known cure, as viable treatments are still under research. Astigmatism, although not presumed connected to these visual disturbances, is a common comorbidity. As well, migraine and tinnitus are common comorbidities which are both associated with a more severe presentation of the syndrome. TMJ may also be a common comorbidity.
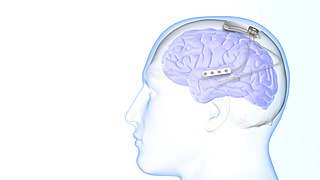
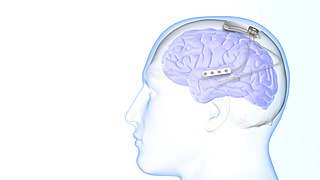
Neurotechnology encompasses any method or electronic device which interfaces with the nervous system to monitor or modulate neural activity.
Tinnitus retraining therapy (TRT) is a form of habituation therapy designed to help people who experience tinnitus—a ringing, buzzing, hissing, or other sound heard when no external sound source is present. Two key components of TRT directly follow from the neurophysiological model of tinnitus: Directive counseling aims to help the sufferer reclassify tinnitus to a category of neutral signals, and sound therapy weakens tinnitus-related neuronal activity.

Vagus nerve stimulation (VNS) is a medical treatment that involves delivering electrical impulses to the vagus nerve. It is used as an add-on treatment for certain types of intractable epilepsy and treatment-resistant depression.
Neurohacking is a subclass of biohacking, focused specifically on the brain. Neurohackers seek to better themselves or others by “hacking the brain” to improve reflexes, learn faster, or treat psychological disorders. The modern neurohacking movement has been around since the 1980s. However, herbal supplements have been used to increase brain function for hundreds of years. After a brief period marked by a lack of research in the area, neurohacking started regaining interest in the early 2000s. Currently, most neurohacking is performed via do-it-yourself (DIY) methods by in-home users.
Thalamocortical dysrhythmia (TCD) is a theoretical framework in which neuroscientists try to explain the positive and negative symptoms induced by neuropsychiatric disorders like Parkinson's Disease, neurogenic pain, tinnitus, visual snow syndrome, schizophrenia, obsessive–compulsive disorder, depressive disorder and epilepsy. In TCD, normal thalamocortical resonance is disrupted by changes in the behaviour of neurons in the thalamus.
TCD can be treated with neurosurgical methods like the central lateral thalamotomy, which due to its invasiveness is only used on patients that have proven resistant to conventional therapies.

A spinal cord stimulator (SCS) or dorsal column stimulator (DCS) is a type of implantable neuromodulation device that is used to send electrical signals to select areas of the spinal cord for the treatment of certain pain conditions. SCS is a consideration for people who have a pain condition that has not responded to more conservative therapy. There are also spinal cord stimulators under research and development that could enable patients with spinal cord injury to walk again via epidural electrical stimulation (EES).
Recurrent thalamo-cortical resonance is an observed phenomenon of oscillatory neural activity between the thalamus and various cortical regions of the brain. It is proposed by Rodolfo Llinas and others as a theory for the integration of sensory information into the whole of perception in the brain. Thalamocortical oscillation is proposed to be a mechanism of synchronization between different cortical regions of the brain, a process known as temporal binding. This is possible through the existence of thalamocortical networks, groupings of thalamic and cortical cells that exhibit oscillatory properties.
Responsive neurostimulation device is a medical device that senses changes in a person's body and uses neurostimulation to respond in the treatment of disease. The FDA has approved devices for use in the United States in the treatment of epileptic seizures and chronic pain conditions. Devices are being studied for use in the treatment of essential tremor, Parkinson's disease, Tourette's syndrome, depression, obesity, and post-traumatic stress disorder.
Neurostimulation is the purposeful modulation of the nervous system's activity using invasive or non-invasive means. Neurostimulation usually refers to the electromagnetic approaches to neuromodulation.
Cortical stimulation mapping (CSM) is a type of electrocorticography that involves a physically invasive procedure and aims to localize the function of specific brain regions through direct electrical stimulation of the cerebral cortex. It remains one of the earliest methods of analyzing the brain and has allowed researchers to study the relationship between cortical structure and systemic function. Cortical stimulation mapping is used for a number of clinical and therapeutic applications, and remains the preferred method for the pre-surgical mapping of the motor cortex and language areas to prevent unnecessary functional damage. There are also some clinical applications for cortical stimulation mapping, such as the treatment of epilepsy.

Restorative neurology is a branch of neurology dedicated to improving functions of the impaired nervous system through selective structural or functional modification of abnormal neurocontrol according to underlying mechanisms and clinically unrecognized residual functions. When impaired, the body naturally reconstructs new neurological pathways and redirects activity. The field of restorative neurology works to accentuate these new pathways and primarily focuses on the theory of the plasticity of an impaired nervous system. Its main goal is to take a broken down and disordered nervous system and return it to a state of normal function. Certain treatment strategies are used to augment instead of fully replace any performance of surviving and also improving the potential of motor neuron functions. This rehabilitation of motor neurons allows patients a therapeutic approach to recovery opposed to physical structural reconstruction. It is applied in a wide range of disorders of the nervous system, including upper motor neuron dysfunctions like spinal cord injury, cerebral palsy, multiple sclerosis and acquired brain injury including stroke, and neuromuscular diseases as well as for control of pain and spasticity. Instead of applying a reconstructive neurobiological approach, i.e. structural modifications, restorative neurology relies on improving residual function. While subspecialties like neurosurgery and pharmacology exist and are useful in diagnosing and treating conditions of the nervous system, restorative neurology takes a pathophysiological approach. Instead of heavily relying on neurochemistry or perhaps an anatomical discipline, restorative neurology encompasses many fields and blends them together.
Neuromodulation is "the alteration of nerve activity through targeted delivery of a stimulus, such as electrical stimulation or chemical agents, to specific neurological sites in the body". It is carried out to normalize – or modulate – nervous tissue function. Neuromodulation is an evolving therapy that can involve a range of electromagnetic stimuli such as a magnetic field (rTMS), an electric current, or a drug instilled directly in the subdural space. Emerging applications involve targeted introduction of genes or gene regulators and light (optogenetics), and by 2014, these had been at minimum demonstrated in mammalian models, or first-in-human data had been acquired. The most clinical experience has been with electrical stimulation.
Ali Rezai is a neurosurgeon interested in the use of brain chip implants in deep brain stimulation and neuromodulation to treat Parkinson's disease, obsessive–compulsive disorder, Alzheimer's disease and traumatic brain injury.

Konstantin Slavin is a Professor and Head of the Department of Stereotactic and functional neurosurgery at the University of Illinois College of Medicine. He is a former president of the American Society for Stereotactic and functional neurosurgery and current vice-president of the World Society for Stereotactic and Functional Neurosurgery. His specialties include Aneurysm, Brain surgery, Brain Tumor, Cerebrovascular Disorders, Craniotomy, Dystonia, Essential Tremor, Facial Nerve Pain, Facial Pain, Glioblastoma, Headache disorders, Laminectomy, Lower back pain, Movement Disorders, Multiple Sclerosis, Neck Pain, Neurosurgery, Neurosurgical Procedures, Pain, Parkinson Disease, Spinal Cord Injuries, and Stroke.
Edward Chang is an American neurosurgeon and scientist. He is the Joan and Sandy Weill Chair of the Department of Neurological Surgery at the University of California, San Francisco and Jeanne Robertson Distinguished Professor.

Alberto Priori is an Italian neurologist, academic, and author. He is a Professor of Neurology at the University of Milan, Director of Neurology 1 Unit at San Paolo Hospital, and the Founder and Coordinator of Aldo Ravelli Center of the University of Milan. He also serves as President of the Neurophysiopatology Tecniques Course, and Professor of Postgraduate Schools - Medicine, Healthcare, Dental Medicine at the same University.