Uterine cancer, also known as womb cancer, includes two types of cancer that develop from the tissues of the uterus. Endometrial cancer forms from the lining of the uterus, and uterine sarcoma forms from the muscles or support tissue of the uterus. Endometrial cancer accounts for approximately 90% of all uterine cancers in the United States. Symptoms of endometrial cancer include changes in vaginal bleeding or pain in the pelvis. Symptoms of uterine sarcoma include unusual vaginal bleeding or a mass in the vagina.

Endometrial cancer is a cancer that arises from the endometrium. It is the result of the abnormal growth of cells that have the ability to invade or spread to other parts of the body. The first sign is most often vaginal bleeding not associated with a menstrual period. Other symptoms include pain with urination, pain during sexual intercourse, or pelvic pain. Endometrial cancer occurs most commonly after menopause.
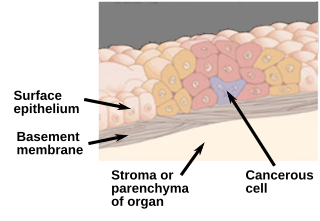
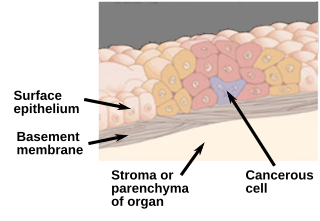
Carcinoma in situ (CIS) is a group of abnormal cells. While they are a form of neoplasm, there is disagreement over whether CIS should be classified as cancer. This controversy also depends on the exact CIS in question. Some authors do not classify them as cancer, however, recognizing that they can potentially become cancer. Others classify certain types as a non-invasive form of cancer. The term "pre-cancer" has also been used.

Endometrioid tumors are a class of tumors that arise in the uterus or ovaries that resemble endometrial glands on histology. They account for 80% of endometrial carcinomas and 20% of malignant ovarian tumors.

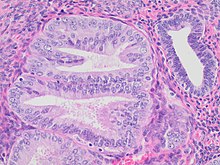
A serous tumour is a neoplasm that typically has papillary to solid formations of tumor cells with crowded nuclei, and which typically arises on the modified Müllerian-derived serous membranes that surround the ovaries in females. Such ovarian tumors are part of the surface epithelial-stromal tumour group of ovarian tumors. They are common neoplasms with a strong tendency to occur bilaterally, and they account for approximately a quarter of all ovarian tumors.

Hyperplasia, or hypergenesis, is an enlargement of an organ or tissue caused by an increase in the amount of organic tissue that results from cell proliferation. It may lead to the gross enlargement of an organ, and the term is sometimes confused with benign neoplasia or benign tumor.

A neoplasm is a type of abnormal and excessive growth of tissue. The process that occurs to form or produce a neoplasm is called neoplasia. The growth of a neoplasm is uncoordinated with that of the normal surrounding tissue, and persists in growing abnormally, even if the original trigger is removed. This abnormal growth usually forms a mass, when it may be called a tumour or tumor.

A benign tumor is a mass of cells (tumor) that does not invade neighboring tissue or metastasize. Compared to malignant (cancerous) tumors, benign tumors generally have a slower growth rate. Benign tumors have relatively well differentiated cells. They are often surrounded by an outer surface or stay contained within the epithelium. Common examples of benign tumors include moles and uterine fibroids.

A precancerous condition is a condition, tumor or lesion involving abnormal cells which are associated with an increased risk of developing into cancer. Clinically, precancerous conditions encompass a variety of abnormal tissues with an increased risk of developing into cancer. Some of the most common precancerous conditions include certain colon polyps, which can progress into colon cancer, monoclonal gammopathy of undetermined significance, which can progress into multiple myeloma or myelodysplastic syndrome. and cervical dysplasia, which can progress into cervical cancer. Bronchial premalignant lesions can progress to squamous cell carcinoma of the lung.

Cowden syndrome is an autosomal dominant inherited condition characterized by benign overgrowths called hamartomas as well as an increased lifetime risk of breast, thyroid, uterine, and other cancers. It is often underdiagnosed due to variability in disease presentation, but 99% of patients report mucocutaneous symptoms by age 20–29. Despite some considering it a primarily dermatologic condition, Cowden's syndrome is a multi-system disorder that also includes neurodevelopmental disorders such as macrocephaly.
The uterine sarcomas form a group of malignant tumors that arises from the smooth muscle or connective tissue of the uterus.

Vulvar intraepithelial neoplasia (VIN) refers to particular changes that can occur in the skin that covers the vulva. VIN is an intraepithelial neoplasia, and can disappear without treatment. VINs are benign but if the changes become more severe, there is a chance of cancer developing after many years, and so it is referred to as a precancerous condition.

Endometrial hyperplasia is a condition of excessive proliferation of the cells of the endometrium, or inner lining of the uterus.

High-grade prostatic intraepithelial neoplasia (HGPIN) is an abnormality of prostatic glands and believed to precede the development of prostate adenocarcinoma.

Uterine serous carcinoma is a malignant form of serous tumor that originates in the uterus. It is an uncommon form of endometrial cancer that typically arises in postmenopausal women. It is typically diagnosed on endometrial biopsy, prompted by post-menopausal bleeding.
Uterine clear-cell carcinoma (CC) is a rare form of endometrial cancer with distinct morphological features on pathology; it is aggressive and has high recurrence rate. Like uterine papillary serous carcinoma CC does not develop from endometrial hyperplasia and is not hormone sensitive, rather it arises from an atrophic endometrium. Such lesions belong to the type II endometrial cancers.
The Bethesda system (TBS), officially called The Bethesda System for Reporting Cervical Cytology, is a system for reporting cervical or vaginal cytologic diagnoses, used for reporting Pap smear results. It was introduced in 1988 and revised in 1991, 2001, and 2014. The name comes from the location of the conference, sponsored by the National Institutes of Health, that established the system.

Bowenoid papulosis is a cutaneous condition characterized by the presence of pigmented verrucous papules on the body of the penis. They are associated with human papillomavirus, the causative agent of genital warts. The lesions have a typical dysplastic histology and are generally considered benign, although a small percentage will develop malignant characteristics.

Villoglandular adenocarcinoma of the cervix is a rare type of cervical cancer that, in relation to other cervical cancers, is typically found in younger women and has a better prognosis.
Microglandular hyperplasia (MGH) of the cervix is an epithelial benign abnormality (lesion) associated with gland proliferation. It can terminate in mature squamous metaplasia, and it is suspected reserve cells are involved in this process, perhaps in the form of reserve cell hyperplasia with glandular differentiation.