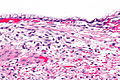
Ovarian mucinous cystadenoma
Mucinous cystadenomas make up 15–20% of all ovarian tumors. They often become very large and can extend up into the abdomen.
These tumors are usually evaluated using ultrasound, CT scan, or MRI. Findings on imaging studies are nonspecific. These ovarian tumors are usually multi-septated, cystic masses with thin walls. They also contain varying amounts of solid tissue which consists of proliferating stromal tissue, papillae, or malignant tumor cells.
Benign mucinous cystadenomas compose 80% of mucinous ovarian tumors [2] and 20–25% of benign ovarian tumors overall. The peak incidence occurs between 30 and 50 years of age. Benign tumors are bilateral in 5–10% of cases.
Types
Pancreatic
Pancreatic mucinous cystadenoma or mucinous cystadenoma of the pancreas (MCN) are a type of mucinous cystic neoplasm of the pancreas. [3] The cure rate is very high in cases on benign cystic lesions, but the case changes if malignant changes ensue. [4] Benign cystadenomas are the most common cystic tumors of the pancreas accounting for 75% of the cases. On average, mucinous accounts for 40–50% of cystic tumors, and serous cystadenoma accounts for 30% of it. Mucinous cystadenomas are in the distal pancreas in about 80% of the cases and distal pancreatectomy is needed for resection. [4] In 20% of the cases it is in the head of the pancreas. [3]
Earlier it was believed that MCN occurs exclusively in women who are middle aged. However, occasional occurrence in men have been reported, [3] especially those who are 45 years of age or above. [5]
Liver
A rare neoplasm, 95% of cases occur in women, especially at the mean age of 45. [6] Biliary cystadenoma and cystadenocarcinoma constitute less than 5% of intrahepatic cysts originating from the bile duct. [6]
Cystadenomas in liver are often confused with hydatid cyst as their appearance on various imaging techniques is nearly same. [7] Treating cystadenomas as hydatid cyst has resulted in recurrence of the cyst. [7]
This page is based on this
Wikipedia article Text is available under the
CC BY-SA 4.0 license; additional terms may apply.
Images, videos and audio are available under their respective licenses.