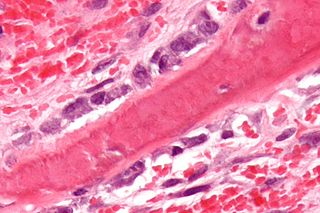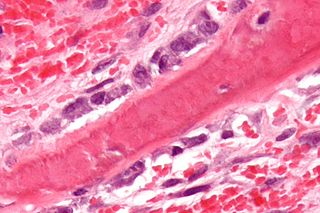
Osteoblasts are cells with a single nucleus that synthesize bone. However, in the process of bone formation, osteoblasts function in groups of connected cells. Individual cells cannot make bone. A group of organized osteoblasts together with the bone made by a unit of cells is usually called the osteon.

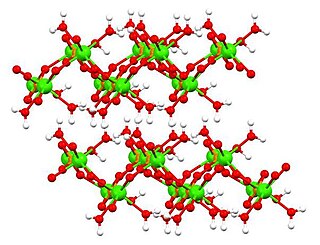
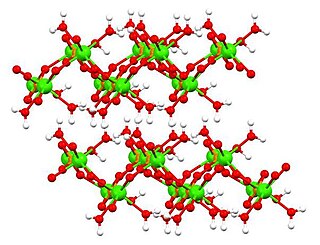
Hydroxyapatite is a naturally occurring mineral form of calcium apatite with the formula Ca5(PO4)3(OH), often written Ca10(PO4)6(OH)2 to denote that the crystal unit cell comprises two entities. It is the hydroxyl endmember of the complex apatite group. The OH− ion can be replaced by fluoride or chloride, producing fluorapatite or chlorapatite. It crystallizes in the hexagonal crystal system. Pure hydroxyapatite powder is white. Naturally occurring apatites can, however, also have brown, yellow, or green colorations, comparable to the discolorations of dental fluorosis.

Bioglass 45S5 or calcium sodium phosphosilicate, is a bioactive glass specifically composed of 45 wt% SiO2, 24.5 wt% CaO, 24.5 wt% Na2O, and 6.0 wt% P2O5. Typical applications of Bioglass 45S5 include: bone grafting biomaterials, repair of periodontal defects, cranial and maxillofacial repair, wound care, blood loss control, stimulation of vascular regeneration, and nerve repair.
Bioactive glasses are a group of surface reactive glass-ceramic biomaterials and include the original bioactive glass, Bioglass. The biocompatibility and bioactivity of these glasses has led them to be used as implant devices in the human body to repair and replace diseased or damaged bones. Most bioactive glasses are silicate-based glasses that are degradable in body fluids and can act as a vehicle for delivering ions beneficial for healing. Bioactive glass is differentiated from other synthetic bone grafting biomaterials, in that it is the only one with anti-infective and angiogenic properties.

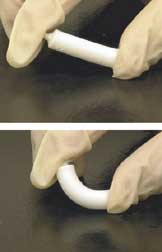
Bone grafting is a surgical procedure that replaces missing bone in order to repair bone fractures that are extremely complex, pose a significant health risk to the patient, or fail to heal properly. Some small or acute fractures can be cured without bone grafting, but the risk is greater for large fractures like compound fractures.

Tricalcium phosphate (sometimes abbreviated TCP), more commonly known as Calcium phosphate, is a calcium salt of phosphoric acid with the chemical formula Ca3(PO4)2. It is also known as tribasic calcium phosphate and bone phosphate of lime (BPL). It is a white solid of low solubility. Most commercial samples of "tricalcium phosphate" are in fact hydroxyapatite.
Dicalcium phosphate is the calcium phosphate with the formula CaHPO4 and its dihydrate. The "di" prefix in the common name arises because the formation of the HPO42– anion involves the removal of two protons from phosphoric acid, H3PO4. It is also known as dibasic calcium phosphate or calcium monohydrogen phosphate. Dicalcium phosphate is used as a food additive, it is found in some toothpastes as a polishing agent and is a biomaterial.

A biomaterial is a substance that has been engineered to interact with biological systems for a medical purpose – either a therapeutic or a diagnostic one. The corresponding field of study, called biomaterials science or biomaterials engineering, is about fifty years old. It has experienced steady growth over its history, with many companies investing large amounts of money into the development of new products. Biomaterials science encompasses elements of medicine, biology, chemistry, tissue engineering and materials science.
Biomimetic materials are materials developed using inspiration from nature. This may be useful in the design of composite materials. Natural structures have inspired and innovated human creations. Notable examples of these natural structures include: honeycomb structure of the beehive, strength of spider silks, bird flight mechanics, and shark skin water repellency. The etymological roots of the neologism "biomimetic" derive from Greek, since bios means "life" and mimetikos means "imitative".
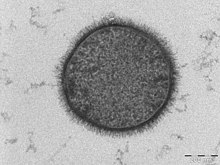
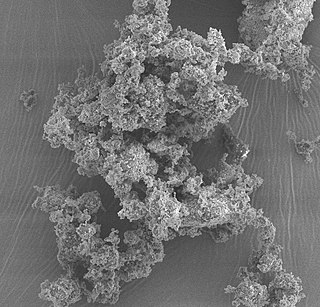
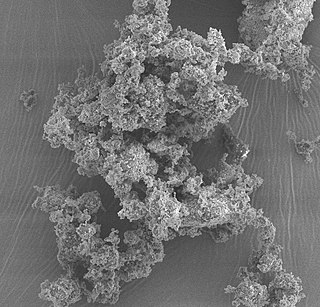
Amorphous calcium phosphate (ACP) is a glassy solid that is formed from the chemical decomposition of a mixture of dissolved phosphate and calcium salts (e.g. (NH4)2HPO4 + Ca(NO3)2). The resulting amorphous mixture consists mostly of calcium and phosphate, but also contains varying amounts of water and hydrogen and hydroxide ions, depending on the synthesis conditions. Such mixtures are also known as calcium phosphate cement.

Bioceramics and bioglasses are ceramic materials that are biocompatible. Bioceramics are an important subset of biomaterials. Bioceramics range in biocompatibility from the ceramic oxides, which are inert in the body, to the other extreme of resorbable materials, which are eventually replaced by the body after they have assisted repair. Bioceramics are used in many types of medical procedures. Bioceramics are typically used as rigid materials in surgical implants, though some bioceramics are flexible. The ceramic materials used are not the same as porcelain type ceramic materials. Rather, bioceramics are closely related to either the body's own materials or are extremely durable metal oxides.
Artificial bone refers to bone-like material created in a laboratory that can be used in bone grafts, to replace human bone that was lost due to severe fractures, disease, etc.
Socket preservation or alveolar ridge preservation is a procedure to reduce bone loss after tooth extraction. After tooth extraction, the jaw bone has a natural tendency to become narrow, and lose its original shape because the bone quickly resorbs, resulting in 30–60% loss in bone volume in the first six months. Bone loss, can compromise the ability to place a dental implant, or its aesthetics and functional ability.

Mineralized tissues are biological tissues that incorporate minerals into soft matrices. Typically these tissues form a protective shield or structural support. Bone, mollusc shells, deep sea sponge Euplectella species, radiolarians, diatoms, antler bone, tendon, cartilage, tooth enamel and dentin are some examples of mineralized tissues.
Octacalcium phosphate (sometimes referred to as OCP) is a form of calcium phosphate with formula Ca8H2(PO4)6·5H2O. OCP may be a precursor to tooth enamel, dentine, and bones. OCP is a precursor of hydroxyapatite (HA), an inorganic biomineral that is important in bone growth. OCP has garnered lots of attention due to its inherent biocompatibility. While OCP exhibits good properties in terms of bone growth, very stringent synthesis requirements make it difficult for mass productions, but nevertheless has shown promise not only in-vitro, but also in in-vivo clinical case studies.
Adsorption is the accumulation and adhesion of molecules, atoms, ions, or larger particles to a surface, but without surface penetration occurring. The adsorption of larger biomolecules such as proteins is of high physiological relevance, and as such they adsorb with different mechanisms than their molecular or atomic analogs. Some of the major driving forces behind protein adsorption include: surface energy, intermolecular forces, hydrophobicity, and ionic or electrostatic interaction. By knowing how these factors affect protein adsorption, they can then be manipulated by machining, alloying, and other engineering techniques to select for the most optimal performance in biomedical or physiological applications.

Biomaterials are materials that are used in contact with biological systems. Biocompatibility and applicability of surface modification with current uses of metallic, polymeric and ceramic biomaterials allow alteration of properties to enhance performance in a biological environment while retaining bulk properties of the desired device.
A simulated body fluid (SBF) is a solution with an ion concentration close to that of human blood plasma, kept under mild conditions of pH and identical physiological temperature. SBF was first introduced by Kokubo et al. in order to evaluate the changes on a surface of a bioactive glass ceramic. Later, cell culture media, in combination with some methodologies adopted in cell culture, were proposed as an alternative to conventional SBF in assessing the bioactivity of materials.
Tetracalcium phosphate is the compound Ca4(PO4)2O, (4CaO·P2O5). It is the most basic of the calcium phosphates, and has a Ca/P ratio of 2, making it the most phosphorus poor phosphate. It is found as the mineral hilgenstockite, which is formed in industrial phosphate rich slag (called "Thomas slag"). This slag was used as a fertiliser due to the higher solubility of tetracalcium phosphate relative to apatite minerals. Tetracalcium phosphate is a component in some calcium phosphate cements that have medical applications.
Crystallopathy is a harmful state or disease associated with the formation and aggregation of crystals in tissues or cavities, or in other words, a heterogeneous group of diseases caused by intrinsic or environmental microparticles or crystals, promoting tissue inflammation and scarring.