Related Research Articles
Obstetrics is the field of study concentrated on pregnancy, childbirth and the postpartum period. As a medical specialty, obstetrics is combined with gynecology under the discipline known as obstetrics and gynecology (OB/GYN), which is a surgical field.

Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is necessary to conclusively diagnose the majority of genetic disorders, with amniocentesis being the gold-standard procedure after 15 weeks' gestation.
Fetal distress, also known as non-reassuring fetal status, is a condition during pregnancy or labor in which the fetus shows signs of inadequate oxygenation. Due to its imprecision, the term "fetal distress" has fallen out of use in American obstetrics. The term "non-reassuring fetal status" has largely replaced it. It is characterized by changes in fetal movement, growth, heart rate, and presence of meconium stained fluid.

Cardiotocography (CTG) is a technique used to monitor the fetal heartbeat and uterine contractions during pregnancy and labour. The machine used to perform the monitoring is called a cardiotocograph.

Placenta praevia is when the placenta attaches inside the uterus but in a position near or over the cervical opening. Symptoms include vaginal bleeding in the second half of pregnancy. The bleeding is bright red and tends not to be associated with pain. Complications may include placenta accreta, dangerously low blood pressure, or bleeding after delivery. Complications for the baby may include fetal growth restriction.

Umbilical cord prolapse is when the umbilical cord comes out of the uterus with or before the presenting part of the baby. The concern with cord prolapse is that pressure on the cord from the baby will compromise blood flow to the baby. It usually occurs during labor but can occur anytime after the rupture of membranes.

Hemolytic disease of the newborn, also known as hemolytic disease of the fetus and newborn, HDN, HDFN, or erythroblastosis fetalis, is an alloimmune condition that develops in a fetus at or around birth, when the IgG molecules produced by the mother pass through the placenta. Among these antibodies are some which attack antigens on the red blood cells in the fetal circulation, breaking down and destroying the cells. The fetus can develop reticulocytosis and anemia. The intensity of this fetal disease ranges from mild to very severe, and fetal death from heart failure can occur. When the disease is moderate or severe, many erythroblasts are present in the fetal blood, earning these forms of the disease the name erythroblastosis fetalis.
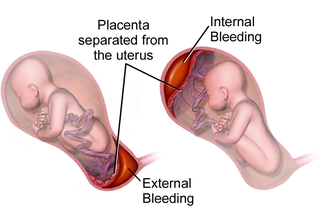
Placental abruption is when the placenta separates early from the uterus, in other words separates before childbirth. It occurs most commonly around 25 weeks of pregnancy. Symptoms may include vaginal bleeding, lower abdominal pain, and dangerously low blood pressure. Complications for the mother can include disseminated intravascular coagulopathy and kidney failure. Complications for the baby can include fetal distress, low birthweight, preterm delivery, and stillbirth.
A contraction stress test (CST) is performed near the end of pregnancy to determine how well the fetus will cope with the contractions of childbirth. The aim is to induce contractions and monitor the fetus to check for heart rate abnormalities using a cardiotocograph. A CST is one type of antenatal fetal surveillance technique.
Postterm pregnancy is when a woman has not yet delivered her baby after 42 weeks of gestation, two weeks beyond the typical 40-week duration of pregnancy. Postmature births carry risks for both the mother and the baby, including fetal malnutrition, meconium aspiration syndrome, and stillbirths. After the 42nd week of gestation, the placenta, which supplies the baby with nutrients and oxygen from the mother, starts aging and will eventually fail. Postterm pregnancy is a reason to induce labor.
Hemolytic disease of the newborn (anti-Kell1) is the second most common cause of severe hemolytic disease of the newborn (HDN) after Rh disease. Anti-Kell1 is becoming relatively more important as prevention of Rh disease is also becoming more effective.

Uterine atony is the failure of the uterus to contract adequately following delivery. Contraction of the uterine muscles during labor compresses the blood vessels and slows flow, which helps prevent hemorrhage and facilitates coagulation. Therefore, a lack of uterine muscle contraction can lead to an acute hemorrhage, as the vasculature is not being sufficiently compressed. Uterine atony is the most common cause of postpartum hemorrhage, which is an emergency and potential cause of fatality. Across the globe, postpartum hemorrhage is among the top five causes of maternal death. Recognition of the warning signs of uterine atony in the setting of extensive postpartum bleeding should initiate interventions aimed at regaining stable uterine contraction.
Placental insufficiency or utero-placental insufficiency is the failure of the placenta to deliver sufficient nutrients to the fetus during pregnancy, and is often a result of insufficient blood flow to the placenta. The term is also sometimes used to designate late decelerations of fetal heart rate as measured by cardiotocography or an NST, even if there is no other evidence of reduced blood flow to the placenta, normal uterine blood flow rate being 600mL/min.

Maternal–fetal medicine (MFM), also known as perinatology, is a branch of medicine that focuses on managing health concerns of the mother and fetus prior to, during, and shortly after pregnancy.
Hemolytic disease of the newborn (anti-RhE) is caused by the anti-RhE antibody of the Rh blood group system. The anti-RhE antibody can be naturally occurring, or arise following immune sensitization after a blood transfusion or pregnancy.

Percutaneous umbilical cord blood sampling (PUBS), also called cordocentesis, fetal blood sampling, or umbilical vein sampling is a diagnostic genetic test that examines blood from the fetal umbilical cord to detect fetal abnormalities. Fetal and maternal blood supply are typically connected in utero with one vein and two arteries to the fetus. The umbilical vein is responsible for delivering oxygen rich blood to the fetus from the mother; the umbilical arteries are responsible for removing oxygen poor blood from the fetus. This allows for the fetus’ tissues to properly perfuse. PUBS provides a means of rapid chromosome analysis and is useful when information cannot be obtained through amniocentesis, chorionic villus sampling, or ultrasound ; this test carries a significant risk of complication and is typically reserved for pregnancies determined to be at high risk for genetic defect. It has been used with mothers with immune thrombocytopenic purpura.

Velamentous cord insertion is a complication of pregnancy where the umbilical cord is inserted in the fetal membranes. It is a major cause of antepartum hemorrhage that leads to loss of fetal blood and associated with high perinatal mortality. In normal pregnancies, the umbilical cord inserts into the middle of the placental mass and is completely encased by the amniotic sac. The vessels are hence normally protected by Wharton's jelly, which prevents rupture during pregnancy and labor. In velamentous cord insertion, the vessels of the umbilical cord are improperly inserted in the chorioamniotic membrane, and hence the vessels traverse between the amnion and the chorion towards the placenta. Without Wharton's jelly protecting the vessels, the exposed vessels are susceptible to compression and rupture.
Fetal scalp blood testing is a technique used in obstetrics during active labor to confirm whether a fetus is receiving enough oxygen. This is a supplementary procedure used to determine if fetal acidemia has occurred following fetal cardiac distress. While continuous fetal heart rate monitoring is the primary method for assessing fetal wellbeing during labor, a change in fetal heart rate is not indicative of fetal acidemia. Some of the signs and symptoms of oxygen deprivation are pH in the umbilical cord, abnormal fetal heartbeat and abnormal coloration of amniotic fluid. This correlation can only be concluded by sampling fetal scalp blood and measuring acid status. Therefore, fetal scalp blood testing could be used to reduce the number of unnecessary emergency caesarean sections made on the decision of fetal heart rate alone.

Fetal electroencephalography, also known as prenatal EEG includes any recording of electrical fluctuations arising from the brain of a fetus. Doctors and scientists use EEGs to detect and characterize brain activity, such as sleep states, potential seizures, or levels of a coma. EEG captures the electrical activity in the vicinity of the recording electrodes. The majority of the neural electrical activity arises from the flow of current from the cell bodies of pyramidal neurons to their apical dendrites, which become depolarized by excitatory inputs from other neurons. To record the most accurate signals, scientists try to minimize the distance between the recording electrode and the neural activity that they want to detect. Given the difficulty of attaching electrodes to a fetus inside a uterus, doctors and scientists use a variety of techniques to record fetal brain activity.

Operative vaginal delivery, also known as assisted or instrumental vaginal delivery, is a vaginal delivery that is assisted by the use of forceps or a vacuum extractor.
References
- ↑ Clark, SL; Gimovsky, ML; Miller, FC (Feb 1, 1984). "The scalp stimulation test: a clinical alternative to fetal scalp blood sampling". American Journal of Obstetrics and Gynecology. 148 (3): 274–7. doi:10.1016/s0002-9378(84)80067-8. PMID 6695974.
- ↑ Skupski, DW; Rosenberg, CR; Eglinton, GS (January 2002). "Intrapartum fetal stimulation tests: a meta-analysis". Obstetrics and Gynecology. 99 (1): 129–34. doi:10.1016/s0029-7844(01)01645-3. PMID 11777523. S2CID 5915067.