Related Research Articles

Cardiotocography (CTG) is a technique used to monitor the fetal heartbeat and the uterine contractions during pregnancy and labour. The machine used to perform the monitoring is called a cardiotocograph.

Placenta praevia is when the placenta attaches inside the uterus but in a position near or over the cervical opening. Symptoms include vaginal bleeding in the second half of pregnancy. The bleeding is bright red and tends not to be associated with pain. Complications may include placenta accreta, dangerously low blood pressure, or bleeding after delivery. Complications for the baby may include fetal growth restriction.
Tocolytics are medications used to suppress premature labor. Preterm birth accounts for 70% of neonatal deaths. Therefore, tocolytic therapy is provided when delivery would result in premature birth, postponing delivery long enough for the administration of glucocorticoids, which accelerate fetal lung maturity but may require one to two days to take effect.
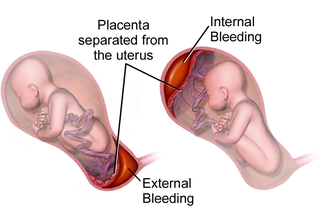
Placental abruption is when the placenta separates early from the uterus, in other words separates before childbirth. It occurs most commonly around 25 weeks of pregnancy. Symptoms may include vaginal bleeding, lower abdominal pain, and dangerously low blood pressure. Complications for the mother can include disseminated intravascular coagulopathy and kidney failure. Complications for the baby can include fetal distress, low birthweight, preterm delivery, and stillbirth.
Antepartum bleeding, also known as antepartum haemorrhage (APH) or prepartum hemorrhage, is genital bleeding during pregnancy after the 28th week of pregnancy up to delivery.
Cervical dilation is the opening of the cervix, the entrance to the uterus, during childbirth, miscarriage, induced abortion, or gynecological surgery. Cervical dilation may occur naturally, or may be induced surgically or medically.

Uterine rupture is when the muscular wall of the uterus tears during pregnancy or childbirth. Symptoms, while classically including increased pain, vaginal bleeding, or a change in contractions, are not always present. Disability or death of the mother or baby may result.

Prelabor rupture of membranes (PROM), previously known as premature rupture of membranes, is breakage of the amniotic sac before the onset of labor. Women usually experience a painless gush or a steady leakage of fluid from the vagina. Complications in the baby may include premature birth, cord compression, and infection. Complications in the mother may include placental abruption and postpartum endometritis.
A nonstress test (NST) is a screening test used in pregnancy to assess fetal status by means of the fetal heart rate and its responsiveness. A cardiotocograph is used to monitor the fetal heart rate and presence or absence of uterine contractions. The test is typically termed "reactive" or "nonreactive".

Prostaglandin E2 (PGE2), also known as dinoprostone, is a naturally occurring prostaglandin with oxytocic properties that is used as a medication. Dinoprostone is used in labor induction, bleeding after delivery, termination of pregnancy, and in newborn babies to keep the ductus arteriosus open. In babies it is used in those with congenital heart defects until surgery can be carried out. It is also used to manage gestational trophoblastic disease. It may be used within the vagina or by injection into a vein.
Postterm pregnancy is when a woman has not yet delivered her baby after 42 weeks of gestation, two weeks beyond the typical 40-week duration of pregnancy. Postmature births carry risks for both the mother and the baby, including fetal malnutrition, meconium aspiration syndrome, and stillbirths. After the 42nd week of gestation, the placenta, which supplies the baby with nutrients and oxygen from the mother, starts aging and will eventually fail. Postterm pregnancy is a reason to induce labor.

Uterine atony is the failure of the uterus to contract adequately following delivery. Contraction of the uterine muscles during labor compresses the blood vessels and slows flow, which helps prevent hemorrhage and facilitates coagulation. Therefore, a lack of uterine muscle contraction can lead to an acute hemorrhage, as the vasculature is not being sufficiently compressed. Uterine atony is the most common cause of postpartum hemorrhage, which is an emergency and potential cause of fatality. Across the globe, postpartum hemorrhage is among the top five causes of maternal death. Recognition of the warning signs of uterine atony in the setting of extensive postpartum bleeding should initiate interventions aimed at regaining stable uterine contraction.
Placental insufficiency or utero-placental insufficiency is the failure of the placenta to deliver sufficient nutrients to the fetus during pregnancy, and is often a result of insufficient blood flow to the placenta. The term is also sometimes used to designate late decelerations of fetal heart rate as measured by cardiotocography or an NST, even if there is no other evidence of reduced blood flow to the placenta, normal uterine blood flow rate being 600mL/min.

A vaginal delivery is the birth of offspring in mammals through the vagina. It is the most common method of childbirth worldwide. It is considered the preferred method of delivery, with lower morbidity and mortality than Caesarean sections (C-sections).

Roberto Caldeyro-Barcia was a Uruguayan doctor who pioneered the field of maternal-fetal medicine, or perinatology. His research with Dr. Hermógenes Alvarez created Montevideo units, a measure of uterine performance during labor. He was a founding editor of the Journal of Perinatal Medicine, a widely published author, a lecturer, and as of 2010 the only Uruguayan to be nominated for a Nobel Prize.
A uterotonic, also known as ecbolic, are pharmacological agents used to induce contraction or greater tonicity of the uterus. Uterotonics are used both to induce labor and to reduce postpartum hemorrhage.
The following outline is provided as an overview of and topical guide to obstetrics:
Uterine Tachysystole is a condition of excessively frequent uterine contractions during pregnancy. It is most often seen in induced or augmented labor, though it can also occur during spontaneous labor, and this may result in fetal hypoxia and acidosis. This may have serious effects on both the mother and the fetus including hemorrhaging and death. There are still major gaps in understanding treatment as well as clinical outcomes of this condition. Uterine tachysystole is defined as more than 5 contractions in 10 minutes, averaged over a 30-minute period.
Locked twins is a rare complication of multiple pregnancy where two fetuses become interlocked during presentation before birth. It occurs in roughly 1 in 1,000 twin deliveries and 1 in 90,000 deliveries overall. Most often, locked twins are delivered via Caesarean section, given that the condition has been diagnosed early enough. The fetal mortality rate is high for the twin that presents first, with over 50% being stillborn.

Prolonged labor is the inability of a woman to proceed with childbirth upon going into labor. Prolonged labor typically lasts over 20 hours for first time mothers, and over 14 hours for women that have already had children. Failure to progress can take place during two different phases; the latent phase and active phase of labor. The latent phase of labor can be emotionally tiring and cause fatigue, but it typically does not result in further problems. The active phase of labor, on the other hand, if prolonged, can result in long term complications.
References
- 1 2 3 4 5 6 Ronald S. Gibbs; et al., eds. (2008). Danforth's obstetrics and gynecology (10th ed.). Philadelphia: Lippincott Williams & Wilkins. p. 161. ISBN 9780781769372.
- ↑ Alan H. DeCherney; T. Murphy Goodwin; et al., eds. (2007). Current diagnosis & treatment : Obstetrics & gynecology (10th ed.). New York: McGraw-Hill. pp. 255. ISBN 978-0-07-143900-8.
- 1 2 3 III, Frances Talaska Fischbach, Marshall Barnett Dunning (2009). A manual of laboratory and diagnostic tests (8th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. pp. 1030–31. ISBN 9780781771948.
- 1 2 3 4 Association of Women's Health, Obstetric, and Neonatal Nurses (2005). Audrey Lyndon; Linda Usher Ali (eds.). Fetal Heart Monitoring: Principles and Practices (3rd ed.). Dubuque, IA: Kendall/Hunt Publishing Co. ISBN 978-0-7575-6234-1.
- ↑ Lagrew DC Jr (March 1995). "The contraction stress test". Clinical Obstetrics and Gynecology. 38 (1): 11–25. doi:10.1097/00003081-199503000-00005. PMID 7796539. S2CID 45260930.
- ↑ Tao Le; et al. (2008). First aid for the family medicine boards . New York: McGraw-Hill Medical. pp. 556. ISBN 978-0-07-159382-3.
- ↑ Munden, ed.: Julie (2005). Professional guide to diagnostic tests. Philadelphia: Lippincott Williams & Wilkins. pp. 682. ISBN 9781582553047.
{{cite book}}:|first=has generic name (help) - 1 2 American College of Obstetricians and Gynecologists (ACOG). (1999). Antepartum fetal surveillance (Practice Bulletin No. 9). Washington, DC: Author.
- 1 2 Evans (2007). Arthur T. (ed.). Manual of obstetrics (7th ed.). Philadelphia: Wolters Kluwer / Lippincott Williams & Wilkins. p. 587. ISBN 9780781796965.
- ↑ Anderson (2005). Jean R. (ed.). A guide to the clinical care of women with HIV (2005 ed.). Rockville, MD: U.S. Dept. of Health & Human Services, Health Resources & Services Administration, HIV/AIDS Bureau. p. 270. ISBN 9780160726118.
- ↑ Ray M, Freeman R, Pine S, Hesselgesser R (September 1972). "Clinical experience with the oxytocin challenge test". Am. J. Obstet. Gynecol. 114 (1): 1–9. doi:10.1016/0002-9378(72)90279-7. PMID 4637035.