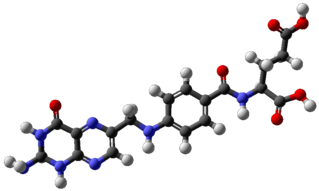
Riboflavin, also known as vitamin B2, is a vitamin found in food and used as a dietary supplement. It is required by the body for cellular respiration. Food sources include eggs, green vegetables, milk and other dairy product, meat, mushrooms, and almonds. Some countries require its addition to grains.

A vitamin is an organic molecule (or a set of molecules closely related chemically, i.e. vitamers) that is an essential micronutrient which an organism needs in small quantities for the proper functioning of its metabolism. Essential nutrients cannot be synthesized in the organism, either at all or not in sufficient quantities, and therefore must be obtained through the diet. Vitamin C can be synthesized by some species but not by others; it is not a vitamin in the first instance but is in the second. The term vitamin does not include the three other groups of essential nutrients: minerals, essential fatty acids, and essential amino acids. Most vitamins are not single molecules, but groups of related molecules called vitamers. For example, there are eight vitamers of vitamin E: four tocopherols and four tocotrienols. Some sources list fourteen vitamins, by including choline, but major health organizations list thirteen: vitamin A (as all-trans-retinol, all-trans-retinyl-esters, as well as all-trans-beta-carotene and other provitamin A carotenoids), vitamin B1 (thiamine), vitamin B2 (riboflavin), vitamin B3 (niacin), vitamin B5 (pantothenic acid), vitamin B6 (pyridoxine), vitamin B7 (biotin), vitamin B9 (folic acid or folate), vitamin B12 (cobalamins), vitamin C (ascorbic acid), vitamin D (calciferols), vitamin E (tocopherols and tocotrienols), and vitamin K (phylloquinone and menaquinones).

Pantothenic acid, also called vitamin B5 is a water-soluble B vitamin and therefore an essential nutrient. All animals require pantothenic acid in order to synthesize coenzyme A (CoA) – essential for fatty acid metabolism – as well as to in general synthesize and metabolize proteins, carbohydrates, and fats.

Vitamin E is a group of eight fat soluble compounds that include four tocopherols and four tocotrienols. Vitamin E deficiency, which is rare and usually due to an underlying problem with digesting dietary fat rather than from a diet low in vitamin E, can cause nerve problems. Vitamin E is a fat-soluble antioxidant protecting cell membranes from reactive oxygen species.
Tocopherols are a class of organic chemical compounds, many of which have vitamin E activity. Because the vitamin activity was first identified in 1936 from a dietary fertility factor in rats, it was named "tocopherol", from the Greek τόκος tókos 'birth' and φέρειν phérein 'to bear or carry', that is "to carry a pregnancy," with the ending "-ol" signifying its status as a chemical alcohol.

Vitamin A is a group of unsaturated nutritional organic compounds that includes retinol, retinal, and several provitamin A carotenoids. Vitamin A has multiple functions: it is important for growth and development, for the maintenance of the immune system, and for good vision. Vitamin A is needed by the retina of the eye in the form of retinal, which combines with protein opsin to form rhodopsin, the light-absorbing molecule necessary for both low-light and color vision. Vitamin A also functions in a very different role as retinoic acid, which is an important hormone-like growth factor for epithelial and other cells.

Retinol, also known as vitamin A1-alcohol, is a vitamin in the vitamin A family found in food and used as a dietary supplement. As a supplement it is ingested to treat and prevent vitamin A deficiency, especially that which results in xerophthalmia. In regions where deficiency is common, a single large dose is recommended to those at high risk a couple of times a year. It is also used to reduce the risk of complications in those who have measles. It is used by mouth or injection into a muscle.
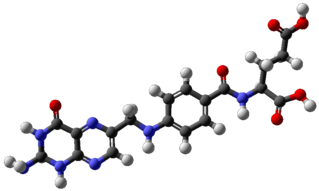
Folate, also known as vitamin B9 and folacin, is one of the B vitamins. Manufactured folic acid, which is converted into folate by the body, is used as a dietary supplement and in food fortification as it is more stable during processing and storage. Folate is required for the body to make DNA and RNA and metabolise amino acids necessary for cell division. As humans cannot make folate, it is required in the diet, making it an essential nutrient. It occurs naturally in many foods. The recommended adult daily intake of folate in the U.S. is 400 micrograms from foods or dietary supplements.
Vitamin deficiency is the condition of a long-term lack of a vitamin. When caused by not enough vitamin intake it is classified as a primary deficiency, whereas when due to an underlying disorder such as malabsorption it is called a secondary deficiency. An underlying disorder may be metabolic – as in a genetic defect for converting tryptophan to niacin – or from lifestyle choices that increase vitamin needs, such as smoking or drinking alcohol. Governments guidelines on vitamin deficiencies advise certain intakes for healthy people, with specific values for women, men, babies, the elderly, and during pregnancy or breastfeeding. Many countries have mandated vitamin food fortification programs to prevent commonly occurring vitamin deficiencies.

A dietary supplement is a manufactured product intended to supplement one's diet by taking a pill, capsule, tablet, powder or liquid. A supplement can provide nutrients either extracted from food sources or that are synthetic in order to increase the quantity of their consumption. The class of nutrient compounds includes vitamins, minerals, fiber, fatty acids and amino acids. Dietary supplements can also contain substances that have not been confirmed as being essential to life, but are marketed as having a beneficial biological effect, such as plant pigments or polyphenols. Animals can also be a source of supplement ingredients, such as collagen from chickens or fish for example. These are also sold individually and in combination, and may be combined with nutrient ingredients. In the United States and Canada, dietary supplements are considered a subset of foods, and are regulated accordingly. The European Commission has also established harmonized rules to help insure that food supplements are safe and properly labeled.

A multivitamin is a preparation intended to serve as a dietary supplement with vitamins, dietary minerals, and other nutritional elements. Such preparations are available in the form of tablets, capsules, pastilles, powders, liquids, or injectable formulations. Other than injectable formulations, which are only available and administered under medical supervision, multivitamins are recognized by the Codex Alimentarius Commission as a category of food.

Vegetarian nutrition is the set of health-related challenges and advantages of vegetarian diets.

Pregnancy, also known as gestation, is the time during which one or more offspring develops inside a woman. A multiple pregnancy involves more than one offspring, such as with twins. Pregnancy usually occurs by sexual intercourse, but can occur through assisted reproductive technology procedures. A pregnancy may end in a live birth, a spontaneous miscarriage, an induced abortion, or a stillbirth. Childbirth typically occurs around 40 weeks from the start of the last menstrual period (LMP). This is just over nine months – where each month averages 31 days. When using fertilization age it is about 38 weeks. An embryo is the developing offspring during the first eight weeks following fertilization, after which, the term fetus is used until birth. Signs and symptoms of early pregnancy may include missed periods, tender breasts, nausea and vomiting, hunger, and frequent urination. Pregnancy may be confirmed with a pregnancy test.

Neural tube defects (NTDs) are a group of birth defects in which an opening in the spine or cranium remains from early in human development. In the third week of pregnancy called gastrulation, specialized cells on the dorsal side of the embryo begin to change shape and form the neural tube. When the neural tube does not close completely, an NTD develops.

Folate deficiency, also known as vitamin B9 deficiency, is a low level of folate and derivatives in the body. Signs of folate deficiency are often subtle. A low number of red blood cells (anemia) is a late finding in folate deficiency and folate deficiency anemia is the term given for this medical condition. It is characterized by the appearance of large-sized, abnormal red blood cells (megaloblasts), which form when there are inadequate stores of folic acid within the body.
Drugs and medications should be avoided while pregnant. Women should speak to their doctor or healthcare professional before starting or stopping any medications while pregnant. Tobacco, alcohol, marijuana, and illicit drug use while pregnant may be dangerous for the unborn baby and may lead to severe health problems and/or birth defects. Even small amounts of alcohol, tobacco, and marijuana have not been proven to be safe when taken while pregnant. In some cases, for example, if the mother has epilepsy or diabetes, the risk of stopping a medication may be worse than risks associated with taking the medication while pregnant. The mother's healthcare professional will help make these decisions about the safest way to protect the health of both the mother and unborn child. In addition to medications and substances, some dietary supplements are important for a healthy pregnancy, however, others may cause harm to the unborn child.
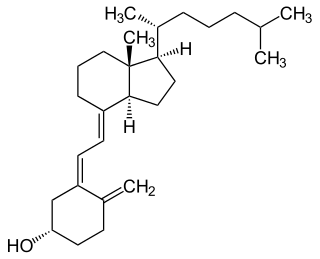
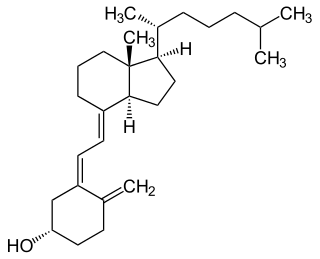
Vitamin D is a group of fat-soluble secosteroids responsible for increasing intestinal absorption of calcium, magnesium, and phosphate, and many other biological effects. In humans, the most important compounds in this group are vitamin D3 (also known as cholecalciferol) and vitamin D2 (ergocalciferol).
Nutriepigenomics is the study of food nutrients and their effects on human health through epigenetic modifications. There is now considerable evidence that nutritional imbalances during gestation and lactation are linked to non-communicable diseases, such as obesity, cardiovascular disease, diabetes, hypertension, and cancer. If metabolic disturbances occur during critical time windows of development, the resulting epigenetic alterations can lead to permanent changes in tissue and organ structure or function and predispose individuals to disease.

Vegan nutrition refers to the nutritional and human health aspects of vegan diets. A well-planned, balanced vegan diet is suitable to meet all recommendations for nutrients in every stage of human life. Vegan diets tend to be higher in dietary fiber, magnesium, folic acid, vitamin C, vitamin E, iron, and phytochemicals; and lower in dietary energy, saturated fat, cholesterol, long-chain omega-3 fatty acids, vitamin D, calcium, zinc, and vitamin B12. Preliminary evidence from epidemiological research indicates that a vegan diet may lower the risk of cancer.
Relatively speaking, the brain consumes an immense amount of energy in comparison to the rest of the body. The mechanisms involved in the transfer of energy from foods to neurons are likely to be fundamental to the control of brain function. Human bodily processes, including the brain, all require both macronutrients, as well as micronutrients.