Related Research Articles

Caesarean section, also known as C-section, cesarean, or caesarean delivery, is the surgical procedure by which one or more babies are delivered through an incision in the mother's abdomen. It is often performed because vaginal delivery would put the mother or child at risk. Reasons for the operation include obstructed labor, twin pregnancy, high blood pressure in the mother, breech birth, shoulder presentation, and problems with the placenta or umbilical cord. A caesarean delivery may be performed based upon the shape of the mother's pelvis or history of a previous C-section. A trial of vaginal birth after C-section may be possible. The World Health Organization recommends that caesarean section be performed only when medically necessary.

Childbirth, also known as labour, parturition and delivery, is the completion of pregnancy where one or more babies exits the internal environment of the mother via vaginal delivery or caesarean section. In 2019, there were about 140.11 million human births globally. In the developed countries, most deliveries occur in hospitals, while in the developing countries most are home births.

The nipple is a raised region of tissue on the surface of the breast from which, in females, milk leaves the breast through the lactiferous ducts to breastfeed an infant. The milk can flow through the nipple passively or it can be ejected by smooth muscle contractions that occur along with the ductal system. Male mammals also have nipples but without the same level of function, and often surrounded by body hair.

Episiotomy, also known as perineotomy, is a surgical incision of the perineum and the posterior vaginal wall generally done by an obstetrician. This is usually performed during the second stage of labor to quickly enlarge the aperture, allowing the baby to pass through. The incision, which can be done from the posterior midline of the vulva straight toward the anus or at an angle to the right or left, is performed under local anesthetic, and is sutured after delivery.

The postpartum period begins after childbirth and is typically considered to last for six weeks. There are three distinct phases of the postnatal period; the acute phase, lasting for six to twelve hours after birth; the subacute phase, lasting six weeks; and the delayed phase, lasting up to six months. During the delayed phase, some changes to the genitourinary system take much longer to resolve and may result in conditions such as urinary incontinence. The World Health Organization (WHO) describes the postnatal period as the most critical and yet the most neglected phase in the lives of mothers and babies; most maternal and newborn deaths occur during this period.
A hysterotomy is an incision made in the uterus. This surgical incision is used in several medical procedures, including during termination of pregnancy in the second trimester and delivering the fetus during caesarean section. It is also used to gain access and perform surgery on a fetus during pregnancy to correct birth defects, and it is an option to achieve resuscitation if cardiac arrest occurs during pregnancy and it is necessary to remove the fetus from the uterus.

Uterine rupture is when the muscular wall of the uterus tears during pregnancy or childbirth. Symptoms, while classically including increased pain, vaginal bleeding, or a change in contractions, are not always present. Disability or death of the mother or baby may result.

Complications of pregnancy are health problems that are related to, or arise during pregnancy. Complications that occur primarily during childbirth are termed obstetric labor complications, and problems that occur primarily after childbirth are termed puerperal disorders. While some complications improve or are fully resolved after pregnancy, some may lead to lasting effects, morbidity, or in the most severe cases, maternal or fetal mortality.

Uterine atony is the failure of the uterus to contract adequately following delivery. Contraction of the uterine muscles during labor compresses the blood vessels and slows flow, which helps prevent hemorrhage and facilitates coagulation. Therefore, a lack of uterine muscle contraction can lead to an acute hemorrhage, as the vasculature is not being sufficiently compressed. Uterine atony is the most common cause of postpartum hemorrhage, which is an emergency and potential cause of fatality. Across the globe, postpartum hemorrhage is among the top five causes of maternal death. Recognition of the warning signs of uterine atony in the setting of extensive postpartum bleeding should initiate interventions aimed at regaining stable uterine contraction.

Postpartum bleeding or postpartum hemorrhage (PPH) is often defined as the loss of more than 500 ml or 1,000 ml of blood following childbirth. Some have added the requirement that there also be signs or symptoms of low blood volume for the condition to exist. Signs and symptoms may initially include: an increased heart rate, feeling faint upon standing, and an increased breathing rate. As more blood is lost, the patient may feel cold, blood pressure may drop, and they may become restless or unconscious. In severe cases circulatory collapse, disseminated intravascular coagulation and death can occur. The condition can occur up to twelve weeks following delivery in the secondary form. The most common cause is poor contraction of the uterus following childbirth. Not all of the placenta being delivered, a tear of the uterus, or poor blood clotting are other possible causes. It occurs more commonly in those who already have a low amount of red blood, are Asian, have a larger fetus or more than one fetus, are obese or are older than 40 years of age. It also occurs more commonly following caesarean sections, those in whom medications are used to start labor, those requiring the use of a vacuum or forceps, and those who have an episiotomy.

Carbetocin, sold under the brand names Pabal among others, is a medication used to prevent excessive bleeding after childbirth, particularly following Cesarean section. It appears to work as well as oxytocin. Due to it being less economical than other options, use is not recommended by NHS Scotland. It is given by injection into a vein or muscle.
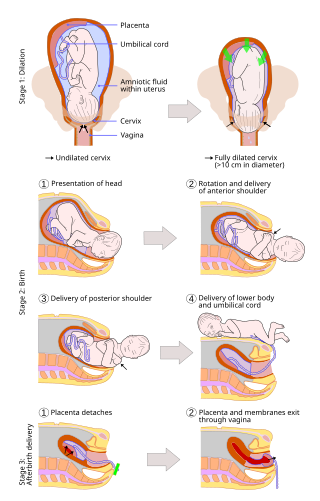
A vaginal delivery is the birth of offspring in mammals through the vagina. It is the most common method of childbirth worldwide. It is considered the preferred method of delivery, as it is correlated with lower morbidity and mortality than caesarean sections (C-sections), though it is not clear whether this is causal.

Breastfeeding, variously known as chestfeeding or nursing, is the process where breast milk is fed to a child. Breast milk may be from the breast, or may be pumped and fed to the infant. The World Health Organization (WHO) recommend that breastfeeding begin within the first hour of a baby's birth and continue as the baby wants. Health organizations, including the WHO, recommend breastfeeding exclusively for six months. This means that no other foods or drinks, other than vitamin D, are typically given. The WHO recommends exclusive breastfeeding for the first 6 months of life, followed by continued breastfeeding with appropriate complementary foods for up to 2 years and beyond. Of the 135 million babies born every year, only 42% are breastfed within the first hour of life, only 38% of mothers practice exclusive breastfeeding during the first six months, and 58% of mothers continue breastfeeding up to the age of two years and beyond.
A postpartum disorder or puerperal disorder is a disease or condition which presents primarily during the days and weeks after childbirth called the postpartum period. The postpartum period can be divided into three distinct stages: the initial or acute phase, 6–12 hours after childbirth; subacute postpartum period, which lasts two to six weeks, and the delayed postpartum period, which can last up to six months. In the subacute postpartum period, 87% to 94% of women report at least one health problem. Long term health problems are reported by 31% of women.
A uterotonic, also known as an oxytocic or ecbolic, is a type of medication used to induce contraction or greater tonicity of the uterus. Uterotonics are used both to induce labor and to reduce postpartum hemorrhage.
Sex after pregnancy is often delayed for several weeks or months, and may be difficult and painful for women. Painful intercourse is the most common sexual activity-related complication after childbirth. Since there are no guidelines on resuming sexual intercourse after childbirth, the postpartum patients are generally advised to resume sex when they feel comfortable to do so. Injury to the perineum or surgical cuts (episiotomy) to the vagina during childbirth can cause sexual dysfunction. Sexual activity in the postpartum period other than sexual intercourse is possible sooner, but some women experience a prolonged loss of sexual desire after giving birth, which may be associated with postnatal depression. Common issues that may last more than a year after birth are greater desire by the man than the woman, and a worsening of the woman's body image.
The following outline is provided as an overview of and topical guide to obstetrics:

Maternal physiological changes in pregnancy are the adaptations that take place during pregnancy that enable the accommodation of the developing embryo and fetus. These are normal physiological adaptations that cause changes in behavior, the functioning of the heart, blood vessels, and blood, metabolism including increases in blood sugar levels, kidney function, posture, and breathing. During pregnancy numerous hormones and proteins are secreted that also have a broad range of effects.

Pain management during childbirth is the partial treatment and a way of reducing any pain that a woman may experience during labor and delivery. The amount of pain a woman feels during labor depends partly on the size and position of her baby, the size of her pelvis, her emotions, the strength of the contractions, and her outlook. Tension increases pain during labor. Virtually all women worry about how they will cope with the pain of labor and delivery. Childbirth is different for each woman and predicting the amount of pain experienced during birth and delivery can not be certain.

Delayed onset of lactation (DOL) describes the absence of copious milk secretion (onset of lactation) within the first 72 hours following childbirth. It affects around 20–40% of lactating women, the prevalence differs among distinct populations.
References
- 1 2 3 Henry 2016, p. 117.
- 1 2 3 4 Davidson 2014, p. 168.
- ↑ The physiological basis of breastfeeding. World Health Organization. 2009.
- 1 2 Henry 2016, p. 120.
- 1 2 Davidson 2014, p. 161.
- ↑ Davidson 2014, p. 162.
- ↑ Lyon 2009.
- ↑ "Stages of labor" . Retrieved 30 July 2017.
- 1 2 Henry 2016, p. 118.
- ↑ Durham 2014, p. 310.
- ↑ Henry 2016, p. 119.
- ↑ Singh & Perfect 2007, pp. 1192–9.
- ↑ Shepherd, Emily; Grivell, Rosalie M. (24 July 2020). "Aspirin (single dose) for perineal pain in the early postpartum period". The Cochrane Database of Systematic Reviews. 2020 (7): CD012129. doi:10.1002/14651858.CD012129.pub3. ISSN 1469-493X. PMC 7388929 . PMID 32702783.
- ↑ Henry 2016, p. 122.
- ↑ Jiang et al. 2017.
- 1 2 Davidson 2014, p. 160.
- ↑ Davidson 2014, p. 163.
- ↑ Steele, Dale W.; Adam, Gaelen P.; Saldanha, Ian J.; Kanaan, Ghid; Zahradnik, Michael L.; Danilack-Fekete, Valery A.; Stuebe, Alison M.; Peahl, Alex F.; Chen, Kenneth K.; Balk, Ethan M. (2023). "Postpartum Home Blood Pressure Monitoring: A Systematic Review". Obstetrics & Gynecology. 142 (2): 285–295. doi: 10.1097/AOG.0000000000005270 . ISSN 0029-7844. PMID 37311173. S2CID 259155390.
- ↑ Davidson 2014, p. 165.
- ↑ Davidson 2014, p. 166.
- ↑ "Should pregnant and breastfeeding women avoid some types of fish?". nhs.uk. 2018-06-27. Retrieved 2018-08-12.