Hyperprolactinaemia is the presence of abnormally high levels of prolactin in the blood. Normal levels average to about 13 ng/mL in women, and 5 ng/mL in men, with an upper normal limit of serum prolactin levels being 15-25 ng/mL for both. When the fasting levels of prolactin in blood exceed this upper limit, hyperprolactinemia is indicated.

Mastitis is inflammation of the breast or udder, usually associated with breastfeeding. Symptoms typically include local pain and redness. There is often an associated fever and general soreness. Onset is typically fairly rapid and usually occurs within the first few months of delivery. Complications can include abscess formation.
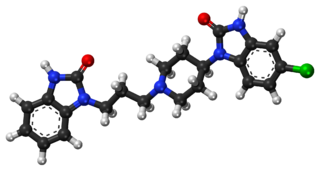
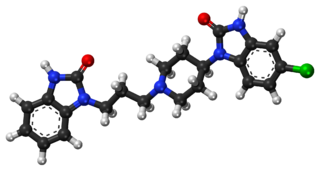
Domperidone, sold under the brand name Motilium among others, is a dopamine antagonist medication which is used to treat nausea and vomiting, certain gastrointestinal problems like gastroparesis, and to induce and promote breast milk production. It may be taken by mouth or rectally.

Breast engorgement occurs in the mammary glands due to expansion and pressure exerted by the synthesis and storage of breast milk. It is also a main factor in altering the ability of the infant to latch-on. Engorgement changes the shape and curvature of the nipple region by making the breast inflexible, flat, hard, and swollen. The nipples on an engorged breast are flat or inverted. Sometimes it may lead to striae on nipples, mainly a preceding symptom of septation mastitis.

Nipple discharge is fluid from the nipple, with or without squeezing the breast. The discharge can be milky, clear, green, purulent, bloody, or faintly yellow. The consistency can be thick, thin, sticky, or watery.
Breast pain is the symptom of discomfort in the breast. Pain that involves both breasts and which occurs repeatedly before the menstrual period is generally not serious. Pain that involves only one part of a breast is more concerning. It is particularly concerning if a hard mass or nipple discharge is also present.
Breast diseases make up a number of conditions. The most common symptoms are a breast mass, breast pain, and nipple discharge.

Breastfeeding difficulties refers to problems that arise from breastfeeding, the feeding of an infant or young child with milk from a woman's breasts. Although babies have a sucking reflex that enables them to suck and swallow milk, and human breast milk is usually the best source of nourishment for human infants, there are circumstances under which breastfeeding can be problematic, or even in rare instances, contraindicated.

Breastfeeding, or nursing, is the process by which human breast milk is fed to a child. Breast milk may be from the breast, or may be expressed by hand or pumped and fed to the infant. The World Health Organization (WHO) recommends that breastfeeding begin within the first hour of a baby's life and continue as often and as much as the baby wants. Health organizations, including the WHO, recommend breastfeeding exclusively for six months. This means that no other foods or drinks, other than vitamin D, are typically given. WHO recommends exclusive breastfeeding for the first 6 months of life, followed by continued breastfeeding with appropriate complementary foods for up to 2 years and beyond. Of the 135 million babies born every year, only 42% are breastfed within the first hour of life, only 38% of mothers practice exclusive breastfeeding during the first six months and 58% of mothers continue breastfeeding up to the age of two years and beyond.
A postpartum disorder or puerperal disorder is a disease or condition which presents primarily during the days and weeks after childbirth called the postpartum period. The postpartum period can be divided into three distinct stages: the initial or acute phase, 6–12 hours after childbirth; subacute postpartum period, which lasts two to six weeks, and the delayed postpartum period, which can last up to six months. In the subacute postpartum period, 87% to 94% of women report at least one health problem. Long term health problems are reported by 31% of women.

A prolactin modulator is a drug which affects the hypothalamic–pituitary–prolactin axis by modulating the secretion of the pituitary hormone prolactin from the anterior pituitary gland. Prolactin inhibitors suppress and prolactin releasers induce the secretion of prolactin, respectively.
The postpartum physiological changes are those expected changes that occur in the woman's body after childbirth, in the postpartum period. These changes mark the beginning of the return of pre-pregnancy physiology and of breastfeeding. Most of the time these postnatal changes are normal and can be managed with medication and comfort measures, but in a few situations complications may develop. Postpartum physiological changes may be different for women delivering by cesarean section. Other postpartum changes, may indicate developing complications such as, postpartum bleeding, engorged breasts, postpartum infections.
Cracked nipple is a condition that can occur in breastfeeding women as a result of a number of possible causes. Developing a cracked nipple can result in soreness, dryness or irritation to, or bleeding of, one or both nipples during breastfeeding. The mother with a cracked nipple can have severe nipple pain when the baby is nursing. This severe pain is a disincentive for continued breastfeeding. The crack can appear as a cut across the tip of the nipple and may extend to its base. Cracked nipple develop after the birth of the infant and is managed with pharmacological and nonpharmacological treatment.
A blocked milk duct is a blockage of one or more ducts carrying milk to the nipple for the purpose of breastfeeding an infant that can cause Mastitis. The symptoms are a tender, localised lump in one breast, with redness in the skin over the lump. The cause of a blocked milk duct is the failure to remove milk from part of the breast. This may be due to infrequent breastfeeding, poor attachment, tight clothing or trauma to the breast. Sometimes the duct to one part of the breast is blocked by thickened milk. A blocked milk duct can be managed by improving the removal of milk and correcting the underlying cause.
In breastfeeding women, low milk supply, also known as lactation insufficiency, insufficient milk syndrome, agalactia, agalactorrhea, hypogalactia or hypogalactorrhea, is the production of breast milk in daily volumes that do not fully meet the nutritional needs of her infant.
Fertility while breastfeeding is controlled by the hormonal effects induced by breastfeeding during the postpartum period. Hormones associated with lactation and breastfeeding can inhibit processes necessary for conception. Because of the high variation of this process, breastfeeding is not recommended to be a method of contraception by medical providers, although correct use of breastfeeding as contraception, termed Lactational Amenorrhea Method (LAM), is as effective as hormonal contraceptive pills for the first six months after birth.

Breastfeeding and mental health is the relationship between postpartum breastfeeding and the mother's and child's mental health. Research indicates breastfeeding may have positive effects on the mother's and child's mental health, though there have been conflicting studies that question the correlation and causation of breastfeeding and maternal mental health. Possible benefits include improved mood and stress levels in the mother, lower risk of postpartum depression, enhanced social emotional development in the child, stronger mother-child bonding and more. Given the benefits of breastfeeding, the World Health Organization (WHO), the European Commission for Public Health (ECPH) and the American Academy of Pediatrics (AAP) suggest exclusive breastfeeding for the first six months of life. Despite these suggestions, estimates indicate 70% of mothers breastfeed their child after birth and 13.5% of infants in the United States are exclusively breastfed. Breastfeeding promotion and support for mothers who are experiencing difficulties or early cessation in breastfeeding is considered a health priority.

Delayed onset of lactation (DOL) describes the absence of copious milk secretion within the first 72 hours following childbirth. It affects around 20-40% of lactating women, the prevalence differs among distinct populations.
Nipple pain is a common symptom of pain at the nipple that occurs in women during breastfeeding after childbirth. The pain shows the highest intensity during the third to the seventh day postpartum and becomes most severe on the third day postpartum.

Establishment of breastfeeding refers to the initiation of providing breast milk of mother to baby. According to the World Health Organisation(WHO), breastfeeding is the best way to provide nourishment, including essential nutrients, energy and antibodies, to infants and toddlers. The start of breastfeeding is supported by the milk production which depends on the development of internal and external breast structure and hormonal control on milk secretion. Besides milk supply, adopting the correct approach of breastfeeding helps build up the maternal bond, which in turn promotes breastfeeding. Not only does nursing strengthen the mother-child relationship, but it also improves the intelligence and immunity of breastfed children and diminishes breastfeeding mothers' risks to have ovarian and breast cancer.