Hemidesmosomes are very small stud-like structures found in keratinocytes of the epidermis of skin that attach to the extracellular matrix. They are similar in form to desmosomes when visualized by electron microscopy, however, desmosomes attach to adjacent cells. Hemidesmosomes are also comparable to focal adhesions, as they both attach cells to the extracellular matrix. Instead of desmogleins and desmocollins in the extracellular space, hemidesmosomes utilize integrins. Hemidesmosomes are found in epithelial cells connecting the basal epithelial cells to the lamina lucida, which is part of the basal lamina. Hemidesmosomes are also involved in signaling pathways, such as keratinocyte migration or carcinoma cell intrusion.

Pemphigus is a rare group of blistering autoimmune diseases that affect the skin and mucous membranes. The name is derived from the Greek root pemphix, meaning "blister".

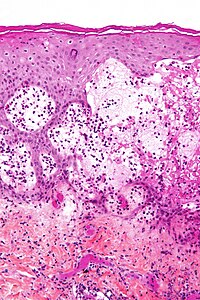
Bullous pemphigoid is an autoimmune pruritic skin disease that typically occurs in people aged over 60, that may involve the formation of blisters (bullae) in the space between the epidermal and dermal skin layers. It is classified as a type II hypersensitivity reaction, which involves formation of anti-hemidesmosome antibodies, causing a loss of keratinocytes to basement membrane adhesion.

Pruritic urticarial papules and plaques of pregnancy (PUPPP), known in United Kingdom as polymorphic eruption of pregnancy (PEP), is a chronic hives-like rash that strikes some women during pregnancy. Some skin changes are known to occur in people who are pregnant while other skin conditions, or dermatoses, that people have prior to getting pregnant will become altered or symptoms will increase. Pruritic urticarial papules and plaques of pregnancy (PUPPP) is one of many skin conditions that is specific to pregnancy and occurs in about 1 in every 160 (0.625%) of pregnancies.

Pemphigus vulgaris is a rare chronic blistering skin disease and the most common form of pemphigus. Pemphigus was derived from the Greek word pemphix, meaning blister. It is classified as a type II hypersensitivity reaction in which antibodies are formed against desmosomes, components of the skin that function to keep certain layers of skin bound to each other. As desmosomes are attacked, the layers of skin separate and the clinical picture resembles a blister. These blisters are due to acantholysis, or breaking apart of intercellular connections through an autoantibody-mediated response. Over time the condition inevitably progresses without treatment: lesions increase in size and distribution throughout the body, behaving physiologically like a severe burn.

Hailey–Hailey disease (HHD), or familial benign chronic pemphigus or familial benign pemphigus, was originally described by the Hailey brothers in 1939. It is a genetic disorder that causes blisters to form on the skin.

Pemphigoid is a group of rare autoimmune blistering diseases of the skin, and mucous membranes. As its name indicates, pemphigoid is similar in general appearance to pemphigus, but, unlike pemphigus, pemphigoid does not feature acantholysis, a loss of connections between skin cells.
Dermatoses of pregnancy are the inflammatory skin diseases that are specific to women while they are pregnant. While some use the term 'polymorphic eruption of pregnancy' to cover these, this term is a synonym used in the UK for Pruritic urticarial papules and plaques of pregnancy, which is the commonest of these skin conditions.

Collagen XVII, previously called BP180, is a transmembrane protein which plays a critical role in maintaining the linkage between the intracellular and the extracellular structural elements involved in epidermal adhesion, identified by Diaz and colleagues in 1990.

Dystonin(DST), also known as bullous pemphigoid antigen 1 (BPAG1), isoforms 1/2/3/4/5/8, is a protein that in humans is encoded by the DST gene.

Dermatitis herpetiformis (DH) is a chronic autoimmune blistering skin condition, characterised by intensely itchy blisters filled with a watery fluid. DH is a cutaneous manifestation of coeliac disease, although the exact causal mechanism is not known. DH is neither related to nor caused by herpes virus; the name means that it is a skin inflammation having an appearance similar to herpes.
Epidermolysis bullosa acquisita, also known as acquired epidermolysis bullosa, is a longterm autoimmune blistering skin disease. It generally presents with fragile skin that blisters and becomes red with or without trauma. Marked scarring is left with thin skin, milia and nail changes. It typically begins around age 50.
Paraneoplastic pemphigus (PNP) is an autoimmune disorder stemming from an underlying tumor. It is hypothesized that antigens associated with the tumor trigger an immune response resulting in blistering of the skin and mucous membranes.
Pruritic folliculitis of pregnancy is a skin condition that occurs in one in 3000 people, about 0.2% of cases, who are in their second to third trimester of pregnancy where the hair follicle becomes inflamed or infected, resulting in a pus filled bump. Some dermatologic conditions aside from pruritic folliculitis during pregnancy include "pruritic urticarial papules and plaques of pregnancy, atopic eruption of pregnancy, pemphigoid gestationis, intrahepatic cholestasis of pregnancy, and pustular psoriasis of pregnancy". This pruritic folliculitis of pregnancy differs from typical pruritic folliculitis; in pregnancy, it is characterized by sterile hair follicles becoming inflamed mainly involving the trunk, contrasting how typical pruritic folliculitis is mainly localized on "the upper back, shoulders, and chest." This condition was first observed after some pregnant individuals showed signs of folliculitis that were different than seen before. The inflammation was thought to be caused by hormonal imbalance, infection from bacteria, fungi, viruses or even an ingrown hair. However, there is no known definitive cause as of yet. These bumps usually begin on the belly and then spread to upper regions of the body as well as the thighs.

Linear IgA bullous dermatosis is a rare immune-mediated blistering skin disease frequently associated with medication exposure, especially vancomycin, with men and women being equally affected. It was first described by Tadeusz Chorzelski in 1979 and may be divided into two types:
A coma blister, or coma bullae, is a skin lesion or blister that typically arises due to pressure in an individual with impaired consciousness. They vary in size, ranging from 4 to 5 centimeters in diameter, and may appear hemorrhagic or blood filled. Coma blisters are usually found in the extremities and trunk. These types of blisters have been associated with the overdose of central nervous system (CNS) depressants especially barbiturates, but also tricyclic antidepressants, hypnotics, benzodiazepines, opiates, antipsychotics, and alcohol. However, studies have found that coma blisters are not caused by the toxicity of these drugs, but due to hypoxia and external pressure on the comatose individual's skin from being immobilized. Coma blisters have been frequently found on individuals who have overdosed on drugs, but have also been found on individuals with chronic kidney failure, hypercalcemia, diabetic ketoacidosis, and a variety of neurologic conditions. Coma blisters are more frequent in adults and less common among children as demonstrated by the few cases published in literature.
Mucous membrane pemphigoid is a rare chronic autoimmune subepithelial blistering disease characterized by erosive lesions of the mucous membranes and skin. It is one of the pemphigoid diseases that can result in scarring.