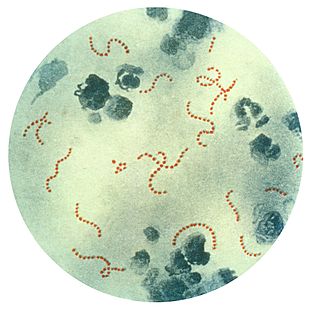
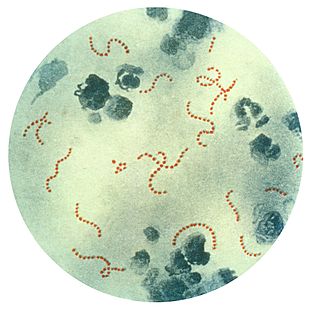
A group A streptococcal infection is an infection with group A streptococcus (GAS). Streptococcus pyogenes comprises the vast majority of the Lancefield group A streptococci, and is often used as a synonym for GAS. However, S. dysgalactiae can also be group A. S. pyogenes is a beta-hemolytic species of Gram positive bacteria that is responsible for a wide range of both invasive and noninvasive infections.

Scarlet fever is a disease resulting from a group A streptococcus infection, also known as Streptococcus pyogenes. The signs and symptoms include a sore throat, fever, headaches, swollen lymph nodes, and a characteristic rash. The rash is red and feels like sandpaper and the tongue may be red and bumpy. It most commonly affects children between five and 15 years of age.

Streptococcal pharyngitis, also known as strep throat, is an infection of the back of the throat including the tonsils caused by group A streptococcus (GAS). Common symptoms include fever, sore throat, red tonsils, and enlarged lymph nodes in the neck. A headache, and nausea or vomiting may also occur. Some develop a sandpaper-like rash which is known as scarlet fever. Symptoms typically begin one to three days after exposure and last seven to ten days.

Neuroleptic malignant syndrome (NMS) is a rare but life-threatening reaction that can occur in response to neuroleptic or antipsychotic medication. Symptoms include high fever, confusion, rigid muscles, variable blood pressure, sweating, and fast heart rate. Complications may include rhabdomyolysis, high blood potassium, kidney failure, or seizures.

Haloperidol, sold under the brand name Haldol among others, is a typical antipsychotic medication. Haloperidol is used in the treatment of schizophrenia, tics in Tourette syndrome, mania in bipolar disorder, delirium, agitation, acute psychosis, and hallucinations in alcohol withdrawal. It may be used by mouth or injection into a muscle or a vein. Haloperidol typically works within 30 to 60 minutes. A long-acting formulation may be used as an injection every four weeks in people with schizophrenia or related illnesses, who either forget or refuse to take the medication by mouth.

Pimozide is an antipsychotic drug of the diphenylbutylpiperidine class. It was discovered at Janssen Pharmaceutica in 1963. It has a high potency compared to chlorpromazine. On a weight basis it is even more potent than haloperidol. It also has special neurologic indications for Tourette syndrome and resistant tics. The side effects include akathisia, tardive dyskinesia, and, more rarely, neuroleptic malignant syndrome and prolongation of the QT interval.

Encephalitis lethargica is an atypical form of encephalitis. Also known as "sleeping sickness" or "sleepy sickness", it was first described in 1917 by the neurologist Constantin von Economo and the pathologist Jean-René Cruchet.

Rheumatic fever (RF) is an inflammatory disease that can involve the heart, joints, skin, and brain. The disease typically develops two to four weeks after a streptococcal throat infection. Signs and symptoms include fever, multiple painful joints, involuntary muscle movements, and occasionally a characteristic non-itchy rash known as erythema marginatum. The heart is involved in about half of the cases. Damage to the heart valves, known as rheumatic heart disease (RHD), usually occurs after repeated attacks but can sometimes occur after one. The damaged valves may result in heart failure, atrial fibrillation and infection of the valves.
Chorea is an abnormal involuntary movement disorder, one of a group of neurological disorders called dyskinesias. The term chorea is derived from the Ancient Greek: χορεία, as the quick movements of the feet or hands are comparable to dancing.
Sydenham's chorea, also known as chorea minor and historically and occasionally referred to as St Vitus' dance, is a disorder characterized by rapid, uncoordinated jerking movements primarily affecting the face, hands and feet. Sydenham's chorea is an autoimmune disease that results from childhood infection with Group A beta-haemolytic Streptococcus. It is reported to occur in 20–30% of people with acute rheumatic fever and is one of the major criteria for it, although it sometimes occurs in isolation. The disease occurs typically a few weeks, but up to 6 months, after the acute infection, which may have been a simple sore throat (pharyngitis).

Hyperkinesia refers to an increase in muscular activity that can result in excessive abnormal movements, excessive normal movements or a combination of both. Hyperkinesia is a state of excessive restlessness which is featured in a large variety of disorders that affect the ability to control motor movement, such as Huntington's disease. It is the opposite of hypokinesia, which refers to decreased bodily movement, as commonly manifested in Parkinson's disease.
A complication in medicine, or medical complication, is an unfavorable result of a disease, health condition, or treatment. Complications may adversely affect the prognosis, or outcome, of a disease. Complications generally involve a worsening in severity of disease or the development of new signs, symptoms, or pathological changes which may become widespread throughout the body and affect other organ systems. Thus, complications may lead to the development of new diseases resulting from a previously existing disease. Complications may also arise as a result of various treatments.
Hemiballismus or hemiballism is a basal ganglia syndrome resulting from damage to the subthalamic nucleus in the basal ganglia. Hemiballismus is a rare hyperkinetic movement disorder, that is characterized by violent involuntary limb movements, on one side of the body, and can cause significant disability. Ballismus affects both sides of the body and is much rarer. Symptoms can decrease during sleep.
Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS) is a hypothesis that there exists a subset of children with rapid onset of obsessive-compulsive disorder (OCD) or tic disorders and these symptoms are caused by group A beta-hemolytic streptococcal (GABHS) infections. The proposed link between infection and these disorders is that an initial autoimmune reaction to a GABHS infection produces antibodies that interfere with basal ganglia function, causing symptom exacerbations. It has been proposed that this autoimmune response can result in a broad range of neuropsychiatric symptoms. The PANDAS hypothesis was based on observations in clinical case studies at the US National Institutes of Health and in subsequent clinical trials where children appeared to have dramatic and sudden OCD exacerbations and tic disorders following infections.
Neuroacanthocytosis is a label applied to several genetic neurological conditions in which the blood contains misshapen, spiculated red blood cells called acanthocytes.
Tourette syndrome is an inherited neurodevelopmental disorder that begins in childhood or adolescence, characterized by the presence of motor and phonic tics. The management of Tourette syndrome has the goal of managing symptoms to achieve optimum functioning, rather than eliminating symptoms; not all persons with Tourette's require treatment, and there is no cure or universally effective medication. Explanation and reassurance alone are often sufficient treatment; education is an important part of any treatment plan.
Arthur K. Shapiro, M.D., was a psychiatrist and expert on Tourette syndrome. His "contributions to the understanding of Tourette syndrome completely changed the prevailing view of this disorder"; he has been described as "the father of modern tic disorder research" and is "revered by his colleagues as the first dean of modern Tourette syndrome researchers".
Tourettism refers to the presence of Tourette-like symptoms in the absence of Tourette syndrome, as the result of other diseases or conditions, known as "secondary causes".
A paraneoplastic syndrome is a syndrome that is the consequence of cancer in the body, specifically due to the production of chemical signaling molecules by tumor cells or by an immune response against the tumor. Unlike a mass effect, it is not due to the local presence of cancer cells.

Basal ganglia disease is a group of physical problems that occur when the group of nuclei in the brain known as the basal ganglia fail to properly suppress unwanted movements or to properly prime upper motor neuron circuits to initiate motor function. Research indicates that increased output of the basal ganglia inhibits thalamocortical projection neurons. Proper activation or deactivation of these neurons is an integral component for proper movement. If something causes too much basal ganglia output, then the ventral anterior (VA) and ventral lateral (VL) thalamocortical projection neurons become too inhibited, and one cannot initiate voluntary movement. These disorders are known as hypokinetic disorders. However, a disorder leading to abnormally low output of the basal ganglia leads to reduced inhibition, and thus excitation, of the thalamocortical projection neurons which synapse onto the cortex. This situation leads to an inability to suppress unwanted movements. These disorders are known as hyperkinetic disorders.