Cause and diagnosis
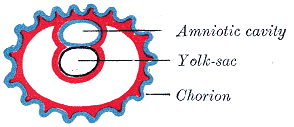
Chorionic hematomas can be caused by the separation of the chorion from the endometrium (inner membrane of the uterus). Hematomas are classified by their location between tissue layers: [4]
- Subchorionic hematomas, the most common type, are between the chorion and endometrium.
- Retroplacental hematomas are entirely behind the placenta and not touching the gestational sac.
- Subamniotic or preplacental hematomas are contained within amnion and chorion. Rare.
Most patients with a small subchorionic hematoma are asymptomatic. [5] Symptoms include vaginal bleeding, abdominal pain, premature labor and threatened miscarriage. [6]
Ultrasonography is the preferred method of diagnosis. [7] A chorionic hematoma appears on ultrasound as a hypoechoic crescent adjacent to the gestational sac. The hematoma is considered small if it is under 20% of the size of the sac and large if it is over 50%. [2]