Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is necessary to conclusively diagnose the majority of genetic disorders, with amniocentesis being the gold-standard procedure after 15 weeks' gestation.
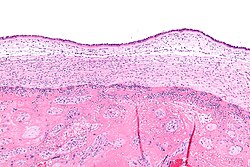
The amniotic sac, also called the bag of waters or the membranes, is the sac in which the embryo and later fetus develops in amniotes. It is a thin but tough transparent pair of membranes that hold a developing embryo until shortly before birth. The inner of these membranes, the amnion, encloses the amniotic cavity, containing the amniotic fluid and the embryo. The outer membrane, the chorion, contains the amnion and is part of the placenta. On the outer side, the amniotic sac is connected to the yolk sac, the allantois, and via the umbilical cord, the placenta.
Fetal distress, also known as non-reassuring fetal status, is a condition during pregnancy or labor in which the fetus shows signs of inadequate oxygenation. Due to its imprecision, the term "fetal distress" has fallen out of use in American obstetrics. The term "non-reassuring fetal status" has largely replaced it. It is characterized by changes in fetal movement, growth, heart rate, and presence of meconium stained fluid.
Oligohydramnios is a medical condition in pregnancy characterized by a deficiency of amniotic fluid, the fluid that surrounds the fetus in the abdomen, in the amniotic sac. The limiting case is anhydramnios, where there is a complete absence of amniotic fluid. It is typically diagnosed by ultrasound when the amniotic fluid index (AFI) measures less than 5 cm or when the single deepest pocket (SDP) of amniotic fluid measures less than 2 cm. Amniotic fluid is necessary to allow for normal fetal movement, lung development, and cushioning from uterine compression. Low amniotic fluid can be attributed to a maternal, fetal, placental or idiopathic cause and can result in poor fetal outcomes including death. The prognosis of the fetus is dependent on the etiology, gestational age at diagnosis, and the severity of the oligohydramnios.

The amniotic fluid is the protective liquid contained by the amniotic sac of a gravid amniote. This fluid serves as a cushion for the growing fetus, but also serves to facilitate the exchange of nutrients, water, and biochemical products between mother and fetus.
Rupture of membranes (ROM) or amniorrhexis is a term used during pregnancy to describe a rupture of the amniotic sac. Normally, it occurs spontaneously at full term either during or at the beginning of labor. Rupture of the membranes is known colloquially as "breaking (one's) water," especially when induced rather than spontaneous, or as one's "water breaking". A premature rupture of membranes (PROM) is a rupture of the amnion that occurs at full term and prior to the onset of labor. In cases of PROM, options include expectant management without intervention, or interventions such as oxytocin or other methods of labor induction, and both are usually accompanied by close monitoring of maternal and fetal health. Preterm premature rupture of membranes (PPROM) is when water breaks both before the onset of labor and before the pregnancy's 37 week gestation. In the United States, more than 120,000 pregnancies per year are affected by a premature rupture of membranes, which is the cause of about one third of preterm deliveries.

Prelabor rupture of membranes (PROM), previously known as premature rupture of membranes, is breakage of the amniotic sac before the onset of labour. Women usually experience a painless gush or a steady leakage of fluid from the vagina. Complications in the baby may include premature birth, cord compression, and infection. Complications in the mother may include placental abruption and postpartum endometritis.

Cervical effacement or cervical ripening refers to the thinning and shortening of the cervix. This process occurs during labor to prepare the cervix for dilation to allow the fetus to pass through the vagina. While this is a normal, physiological process that occurs at the later end of pregnancy, it can also be induced through medications and procedures.

Group B streptococcal infection, also known as Group B streptococcal disease or just Group B strep infection, is the infectious disease caused by the bacterium Streptococcus agalactiae. Streptococcus agalactiae is the most common human pathogen belonging to group B of the Lancefield classification of streptococci—hence the name of group B stretococcal (GBS). Infection with GBS can cause serious illness and sometimes death, especially in newborns, the elderly, and people with compromised immune systems. The most severe form of group B streptococcal disease is neonatal meningitis in infants, which is frequently lethal and can cause permanent neuro-cognitive impairment.
In obstetrics, asynclitic birth, or asynclitism, refers to the malposition of the fetal head in the uterus relative to the birth canal. Many babies enter the pelvis in an asynclitic presentation, but in most cases, the issue is corrected during labor. Asynclitic presentation is not the same as shoulder presentation, where the shoulder enters first.

Velamentous cord insertion is a complication of pregnancy where the umbilical cord is inserted in the fetal membranes. It is a major cause of antepartum hemorrhage that leads to loss of fetal blood and associated with high perinatal mortality. In normal pregnancies, the umbilical cord inserts into the middle of the placental mass and is completely encased by the amniotic sac. The vessels are hence normally protected by Wharton's jelly, which prevents rupture during pregnancy and labor. In velamentous cord insertion, the vessels of the umbilical cord are improperly inserted in the chorioamniotic membrane, and hence the vessels traverse between the amnion and the chorion towards the placenta. Without Wharton's jelly protecting the vessels, the exposed vessels are susceptible to compression and rupture.
An obstetric labor complication is a difficulty or abnormality that arises during the process of labor or delivery.
Placental alpha microglobulin-1 (PAMG-1) is a human protein that was first isolated in 1975 from amniotic fluid. PAMG-1 is an important biomarker for the detection of premature rupture of fetal membrane (PROM) The high concentration of PAMG-1 in amniotic fluid means it can be used to detect if this fluid is present in the cervico-vaginal discharge of pregnant women; the presence of PAMG-1 in the discharge suggests that amniotic fluid is present, and therefore suggests that PROM has occurred. PAMG-1 was originally referred to as specific alpha-1 globulin of placenta.

The fetal membranes are the four extraembryonic membranes, associated with the developing embryo, and fetus in humans and other mammals. They are the amnion, chorion, allantois, and yolk sac. The amnion and the chorion are the chorioamniotic membranes that make up the amniotic sac which surrounds and protects the embryo. The fetal membranes are four of six accessory organs developed by the conceptus that are not part of the embryo itself, the other two are the placenta, and the umbilical cord.

Circumvallate placenta is a rare condition affecting about 1-2% of pregnancies, in which the amnion and chorion fetal membranes essentially "double back" on the fetal side around the edges of the placenta. After delivery, a circumvallate placenta has a thick ring of membranes on its fetal surface. Circumvallate placenta is a placental morphological abnormality associated with increased fetal morbidity and mortality due to the restricted availability of nutrients and oxygen to the developing fetus.
Amnioinfusion is a method in which isotonic fluid is instilled into the uterine cavity.
Neonatal sepsis is a type of neonatal infection and specifically refers to the presence in a newborn baby of a bacterial blood stream infection (BSI) in the setting of fever. Older textbooks may refer to neonatal sepsis as "sepsis neonatorum". Criteria with regards to hemodynamic compromise or respiratory failure are not useful clinically because these symptoms often do not arise in neonates until death is imminent and unpreventable. Neonatal sepsis is divided into two categories: early-onset sepsis (EOS) and late-onset sepsis (LOS). EOS refers to sepsis presenting in the first 7 days of life, with LOS referring to presentation of sepsis after 7 days. Neonatal sepsis is the single most common cause of neonatal death in hospital as well as community in developing country.
Artificial rupture of membranes (AROM), also known as an amniotomy, is performed by a midwife or obstetrician and was once thought to be an effective means to induce or accelerate labor. The membranes can be ruptured using a specialized tool, such as an amnihook or amnicot, or they may be ruptured by the proceduralist's finger. The different techniques for artificial rupture of membranes have not been extensively compared in the literature. In one study comparing amnihook versus amnicot for artificial rupture of membranes, use of an amnicot was associated with fewer neonatal scalp lacerations.

Neonatal infections are infections of the neonate (newborn) acquired during prenatal development or within the first four weeks of life. Neonatal infections may be contracted by mother to child transmission, in the birth canal during childbirth, or after birth. Neonatal infections may present soon after delivery, or take several weeks to show symptoms. Some neonatal infections such as HIV, hepatitis B, and malaria do not become apparent until much later. Signs and symptoms of infection may include respiratory distress, temperature instability, irritability, poor feeding, failure to thrive, persistent crying and skin rashes.

Operative vaginal delivery, also known as assisted or instrumental vaginal delivery, is a vaginal delivery that is assisted by the use of forceps or a vacuum extractor.