The endometrium is the inner epithelial layer, along with its mucous membrane, of the mammalian uterus. It has a basal layer and a functional layer: the basal layer contains stem cells which regenerate the functional layer. The functional layer thickens and then is shed during menstruation in humans and some other mammals, including apes, Old World monkeys, some species of bat, the elephant shrew and the Cairo spiny mouse. In most other mammals, the endometrium is reabsorbed in the estrous cycle. During pregnancy, the glands and blood vessels in the endometrium further increase in size and number. Vascular spaces fuse and become interconnected, forming the placenta, which supplies oxygen and nutrition to the embryo and fetus. The speculated presence of an endometrial microbiota has been argued against.
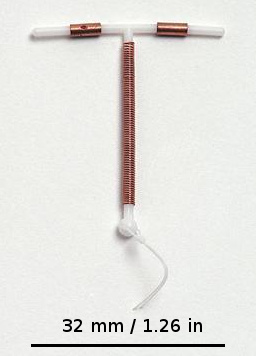
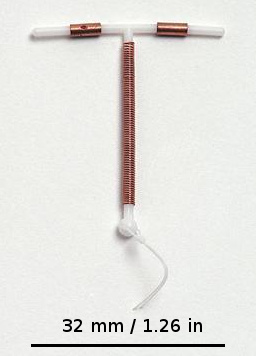
A copper intrauterine device (IUD), also known as an intrauterine coil or copper coil or non-hormonal IUD, is a type of intrauterine device which contains copper. It is used for birth control and emergency contraception within five days of unprotected sex. It is one of the most effective forms of birth control with a one-year failure rate around 0.7%. The device is placed in the uterus and lasts up to twelve years. It may be used by women of all ages regardless of whether or not they have had children. Following removal, fertility quickly returns.

Pelvic inflammatory disease, also known as pelvic inflammatory disorder (PID), is an infection of the upper part of the female reproductive system, namely the uterus, fallopian tubes, and ovaries, and inside of the pelvis. Often, there may be no symptoms. Signs and symptoms, when present, may include lower abdominal pain, vaginal discharge, fever, burning with urination, pain with sex, bleeding after sex, or irregular menstruation. Untreated PID can result in long-term complications including infertility, ectopic pregnancy, chronic pelvic pain, and cancer.

Ectopic pregnancy is a complication of pregnancy in which the embryo attaches outside the uterus. Signs and symptoms classically include abdominal pain and vaginal bleeding, but fewer than 50 percent of affected women have both of these symptoms. The pain may be described as sharp, dull, or crampy. Pain may also spread to the shoulder if bleeding into the abdomen has occurred. Severe bleeding may result in a fast heart rate, fainting, or shock. With very rare exceptions, the fetus is unable to survive.

Miscarriage, also known in medical terms as a spontaneous abortion, is the death and expulsion of an embryo or fetus before it can survive independently. The term miscarriage is sometimes used to refer to all forms of pregnancy loss and pregnancy with abortive outcomes before 20 weeks of gestation.

A pregnancy test is used to determine whether a female is pregnant or not. The two primary methods are testing for the female pregnancy hormone in blood or urine using a pregnancy test kit, and scanning with ultrasonography. Testing blood for hCG results in the earliest detection of pregnancy. Almost all pregnant women will have a positive urine pregnancy test one week after the first day of a missed menstrual period.

Adenomyosis is a medical condition characterized by the growth of cells that proliferate on the inside of the uterus (endometrium) atypically located among the cells of the uterine wall (myometrium), as a result, thickening of the uterus occurs. As well as being misplaced in patients with this condition, endometrial tissue is completely functional. The tissue thickens, sheds and bleeds during every menstrual cycle.

Gynecologic ultrasonography or gynecologic sonography refers to the application of medical ultrasonography to the female pelvic organs as well as the bladder, the adnexa, and the recto-uterine pouch. The procedure may lead to other medically relevant findings in the pelvis.This technique is useful to detect myomas or mullerian malformations.

A hormonal intrauterine device (IUD), also known as an intrauterine system (IUS) with progestogen and sold under the brand name Mirena among others, is an intrauterine device that releases a progestogenic hormonal agent such as levonorgestrel into the uterus. It is used for birth control, heavy menstrual periods, and to prevent excessive build of the lining of the uterus in those on estrogen replacement therapy. It is one of the most effective forms of birth control with a one-year failure rate around 0.2%. The device is placed in the uterus and lasts three to eight years. Fertility often returns quickly following removal.

An abdominal pregnancy is a rare type of ectopic pregnancy where the embryo or fetus is growing and developing outside the uterus, in the abdomen, and not in a fallopian tube, an ovary, or the broad ligament.
Adenomyoma is a tumor (-oma) including components derived from glands (adeno-) and muscle (-my-). It is a type of complex and mixed tumor, and several variants have been described in the medical literature. Uterine adenomyoma, the localized form of uterine adenomyosis, is a tumor composed of endometrial gland tissue and smooth muscle in the myometrium. Adenomyomas containing endometrial glands are also found outside of the uterus, most commonly on the uterine adnexa but can also develop at distant sites outside of the pelvis. Gallbladder adenomyoma, the localized form of adenomyomatosis, is a polypoid tumor in the gallbladder composed of hyperplastic mucosal epithelium and muscularis propria.

A hydrosalpinx is a condition that occurs when a fallopian tube is blocked and fills with serous or clear fluid near the ovary. The blocked tube may become substantially distended giving the tube a characteristic sausage-like or retort-like shape. The condition is often bilateral and the affected tubes may reach several centimeters in diameter. The blocked tubes cause infertility. A fallopian tube filled with blood is a hematosalpinx, and with pus a pyosalpinx.

An interstitial pregnancy is a uterine but ectopic pregnancy; the pregnancy is located outside the uterine cavity in that part of the fallopian tube that penetrates the muscular layer of the uterus. The term cornual pregnancy is sometimes used as a synonym, but remains ambiguous as it is also applied to indicate the presence of a pregnancy located within the cavity in one of the two upper "horns" of a bicornuate uterus. Interstitial pregnancies have a higher mortality than ectopics in general.

A cervical pregnancy is an ectopic pregnancy that has implanted in the uterine endocervix. Such a pregnancy typically aborts within the first trimester, however, if it is implanted closer to the uterine cavity – a so-called cervico-isthmic pregnancy – it may continue longer. Placental removal in a cervical pregnancy may result in major hemorrhage.
Ovarian pregnancy refers to an ectopic pregnancy that is located in the ovary. Typically the egg cell is not released or picked up at ovulation, but fertilized within the ovary where the pregnancy implants. Such a pregnancy usually does not proceed past the first four weeks of pregnancy. An untreated ovarian pregnancy causes potentially fatal intra-abdominal bleeding and thus may become a medical emergency.

Fertility testing is the process by which fertility is assessed, both generally and also to find the "fertile window" in the menstrual cycle. General health affects fertility, and STI testing is an important related field.
Early pregnancy bleeding refers to vaginal bleeding before 14 weeks of gestational age. If the bleeding is significant, hemorrhagic shock may occur. Concern for shock is increased in those who have loss of consciousness, chest pain, shortness of breath, or shoulder pain.
Endometriosis and its complications are a major cause of female infertility. Endometriosis is a dysfunction characterized by the migration of endometrial tissue to areas outside of the endometrium of the uterus. The most common places to find stray tissue are on ovaries and fallopian tubes, followed by other organs in the lower abdominal cavity such as the bladder and intestines. Typically, the endometrial tissue adheres to the exteriors of the organs, and then creates attachments of scar tissue called adhesions that can join adjacent organs together. The endometrial tissue and the adhesions can block a fallopian tube and prevent the meeting of ovum and sperm cells, or otherwise interfere with fertilization, implantation and, rarely, the carrying of the fetus to term.
Repeated implantation failure (RIF) is the repeated failure of the embryo to implant onto the side of the uterus wall following IVF treatment. Implantation happens at 6–7 days after conception and involves the embedding of the growing embryo into the mothers uterus and a connection being formed. A successful implantation can be determined by using an ultrasound to view the sac which the baby grows in, inside the uterus.
Pregnancy in a rudimentary horn of the uterus is a very rare type of ectopic pregnancy. This type of pregnancy can be life-threatening, as the rudimentary horn is not meant to sustain a pregnancy and is at risk of rupturing.