The placenta is a temporary embryonic and later fetal organ that begins developing from the blastocyst shortly after implantation. It plays critical roles in facilitating nutrient, gas and waste exchange between the physically separate maternal and fetal circulations, and is an important endocrine organ, producing hormones that regulate both maternal and fetal physiology during pregnancy. The placenta connects to the fetus via the umbilical cord, and on the opposite aspect to the maternal uterus in a species-dependent manner. In humans, a thin layer of maternal decidual (endometrial) tissue comes away with the placenta when it is expelled from the uterus following birth. Placentas are a defining characteristic of placental mammals, but are also found in marsupials and some non-mammals with varying levels of development.

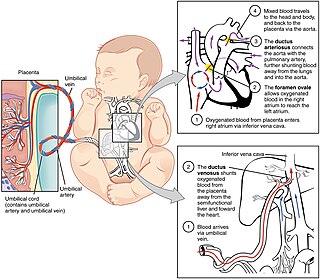
In placental mammals, the umbilical cord is a conduit between the developing embryo or fetus and the placenta. During prenatal development, the umbilical cord is physiologically and genetically part of the fetus and normally contains two arteries and one vein, buried within Wharton's jelly. The umbilical vein supplies the fetus with oxygenated, nutrient-rich blood from the placenta. Conversely, the fetal heart pumps low-oxygen, nutrient-depleted blood through the umbilical arteries back to the placenta.

A breech birth is when a baby is born bottom first instead of head first, as is normal. Around 3–5% of pregnant women at term have a breech baby. Due to their higher than average rate of possible complications for the baby, breech births are generally considered higher risk. Breech births also occur in many other mammals such as dogs and horses, see veterinary obstetrics.

The umbilical vein is a vein present during fetal development that carries oxygenated blood from the placenta into the growing fetus. The umbilical vein provides convenient access to the central circulation of a neonate for restoration of blood volume and for administration of glucose and drugs.

Twin-to-twin transfusion syndrome (TTTS), also known as feto-fetal transfusion syndrome (FFTS), twin oligohydramnios-polyhydramnios sequence (TOPS) and stuck twin syndrome, is a complication of monochorionic multiple pregnancies in which there is disproportionate blood supply between the fetuses. This leads to unequal levels of amniotic fluid between each fetus and usually leads to death of the undersupplied twin and, without treatment, usually death or a range of birth defects or disabilities for a surviving twin, such as underdeveloped, damaged or missing limbs, digits or organs, especially cerebral palsy.
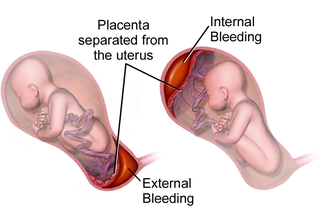
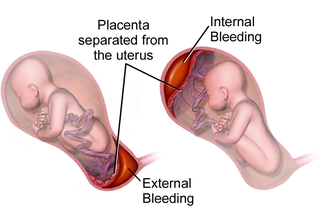
Placental abruption is when the placenta separates early from the uterus, in other words separates before childbirth. It occurs most commonly around 25 weeks of pregnancy. Symptoms may include vaginal bleeding, lower abdominal pain, and dangerously low blood pressure. Complications for the mother can include disseminated intravascular coagulopathy and kidney failure. Complications for the baby can include fetal distress, low birthweight, preterm delivery, and stillbirth.
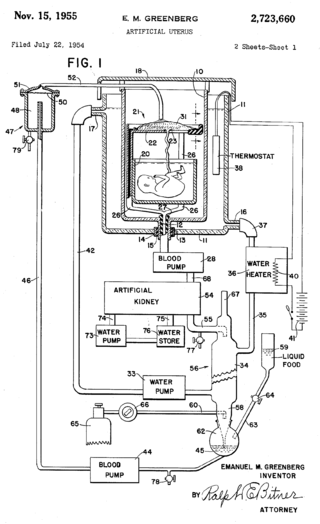
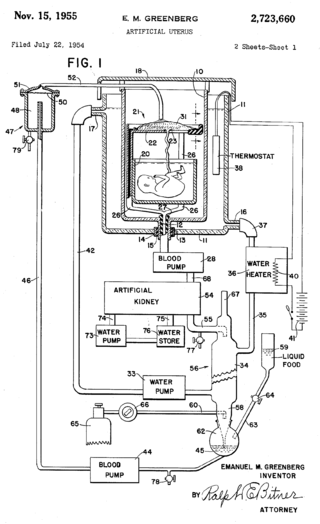
An artificial womb or artificial uterus is a device that would allow for extracorporeal pregnancy, by growing a fetus outside the body of an organism that would normally carry the fetus to term. An artificial uterus, as a replacement organ, would have many applications. It could be used to assist male or female couples in the development of a fetus. This can potentially be performed as a switch from a natural uterus to an artificial uterus, thereby moving the threshold of fetal viability to a much earlier stage of pregnancy. In this sense, it can be regarded as a neonatal incubator with very extended functions. It could also be used for the initiation of fetal development. An artificial uterus could also help make fetal surgery procedures at an early stage an option instead of having to postpone them until term of pregnancy.
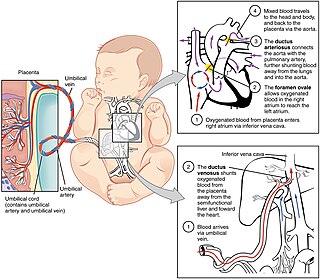
In humans, the circulatory system is different before and after birth. The fetal circulation is composed of the placenta, umbilical blood vessels encapsulated by the umbilical cord, heart and systemic blood vessels. A major difference between the fetal circulation and postnatal circulation is that the lungs are not used during the fetal stage resulting in the presence of shunts to move oxygenated blood and nutrients from the placenta to the fetal tissue. At birth, the start of breathing and the severance of the umbilical cord prompt various changes that quickly transform fetal circulation into postnatal circulation.

Fetal surgery, also known as antenatal surgery or prenatal surgery, is a growing branch of maternal-fetal medicine that covers any of a broad range of surgical techniques that are used to treat congenital abnormalities in fetuses who are still in the pregnant uterus. There are three main types: open fetal surgery, which involves completely opening the uterus to operate on the fetus; minimally invasive fetoscopic surgery, which uses small incisions and is guided by fetoscopy and sonography; and percutaneous fetal therapy, which involves placing a catheter under continuous ultrasound guidance.
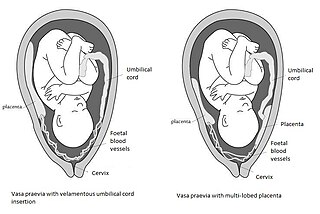
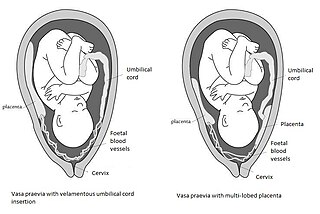
Vasa praevia is a condition in which fetal blood vessels cross or run near the internal opening of the uterus. These vessels are at risk of rupture when the supporting membranes rupture, as they are unsupported by the umbilical cord or placental tissue.
In obstetrics, asynclitic birth, or asynclitism, refers to the malposition of the fetal head in the uterus relative to the birth canal. Many babies enter the pelvis in an asynclitic presentation, but in most cases, the issue is corrected during labor. Asynclitic presentation is not to be confused with a shoulder presentation, where the shoulder leads first.

Velamentous cord insertion is a complication of pregnancy where the umbilical cord is inserted in the fetal membranes. It is a major cause of antepartum hemorrhage that leads to loss of fetal blood and associated with high perinatal mortality. In normal pregnancies, the umbilical cord inserts into the middle of the placental mass and is completely encased by the amniotic sac. The vessels are hence normally protected by Wharton's jelly, which prevents rupture during pregnancy and labor. In velamentous cord insertion, the vessels of the umbilical cord are improperly inserted in the chorioamniotic membrane, and hence the vessels traverse between the amnion and the chorion towards the placenta. Without Wharton's jelly protecting the vessels, the exposed vessels are susceptible to compression and rupture.
An obstetric labor complication is a difficulty or abnormality that arises during the process of labor or delivery.

Congenital pulmonary airway malformation (CPAM), formerly known as congenital cystic adenomatoid malformation (CCAM), is a congenital disorder of the lung similar to bronchopulmonary sequestration. In CPAM, usually an entire lobe of lung is replaced by a non-working cystic piece of abnormal lung tissue. This abnormal tissue will never function as normal lung tissue. The underlying cause for CPAM is unknown. It occurs in approximately 1 in every 30,000 pregnancies.

Circumvallate placenta is a rare condition affecting about 1-2% of pregnancies, in which the amnion and chorion fetal membranes essentially "double back" on the fetal side around the edges of the placenta. After delivery, a circumvallate placenta has a thick ring of membranes on its fetal surface. Circumvallate placenta is a placental morphological abnormality associated with increased fetal morbidity and mortality due to the restricted availability of nutrients and oxygen to the developing fetus.
Amnioinfusion is a method in which isotonic fluid is instilled into the uterine cavity.

Placental expulsion occurs when the placenta comes out of the birth canal after childbirth. The period of time starting just after the baby is expelled until just after the placenta is expelled is called the third stage of labor.

Emergency childbirth is the precipitous birth of an infant in an unexpected setting. In planned childbirth, mothers choose the location and obstetric team ahead of time. Options range from delivering at home, at a hospital, a medical facility or a birthing center. Sometimes, birth can occur on the way to these facilities, without a healthcare team. The rates of unplanned childbirth are low. If the birth is imminent, emergency measures may be needed. Emergency services can be contacted for help in some countries.
The anomaly scan, also sometimes called the anatomy scan, 20-week ultrasound, or level 2 ultrasound, evaluates anatomic structures of the fetus, placenta, and maternal pelvic organs. This scan is an important and common component of routine prenatal care. The function of the ultrasound is to measure the fetus so that growth abnormalities can be recognized quickly later in pregnancy, to assess for congenital malformations and multiple pregnancies, and to plan method of delivery.

Pulmonary agenesis is an inborn lung underdevelopment that is rare and potentially lethal. The disorder is caused by a complete developmental arrest of the primitive lung during embryonic life, and it is often associated with other developmental defects. Bilateral and unilateral pulmonary agenesis are classified, depending on whether one side of the lung or both sides are affected. Bilateral pulmonary agenesis is lethal, while the mortality rate of unilateral pulmonary agenesis is higher than 50%. Depending on the severity, the symptom ranges from none to various respiratory complaints. It is detectable prenatally, however, its nonspecific clinical features act as the obstacle for diagnosing. The exact cause of pulmonary agenesis is still obscure. However, theories have been raised regarding the vascular, iatrogenic, viral and genetic causes of pulmonary agenesis in an attempt to explain the pathogenesis of the disorder. In most cases of pulmonary agenesis, surgical resection is performed to remove the malformed lobe or the entire defected lung of the patient depending on the severity of the respiratory impairment.