Related Research Articles

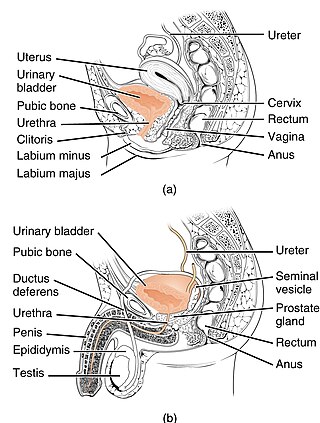
Urination is the release of urine from the bladder to the outside of the body. Urine is released through the urethra and exits the penis or vulva through the urinary meatus in placental mammals, but is released through the cloaca in other vertebrates. It is the urinary system's form of excretion. It is also known medically as micturition, voiding, uresis, or, rarely, emiction, and known colloquially by various names including peeing, weeing, pissing, and euphemistically number one. The process of urination is under voluntary control in healthy humans and other animals, but may occur as a reflex in infants, some elderly individuals, and those with neurological injury. It is normal for adult humans to urinate up to seven times during the day.
Urinary incontinence (UI), also known as involuntary urination, is any uncontrolled leakage of urine. It is a common and distressing problem, which may have a large impact on quality of life. Urinary incontinence is common in older women and has been identified as an important issue in geriatric health care. The term enuresis is often used to refer to urinary incontinence primarily in children, such as nocturnal enuresis. UI is an example of a stigmatized medical condition, which creates barriers to successful management and makes the problem worse. People may be too embarrassed to seek medical help, and attempt to self-manage the symptom in secrecy from others.

Nocturnal enuresis (NE), also informally called bedwetting, is involuntary urination while asleep after the age at which bladder control usually begins. Bedwetting in children and adults can result in emotional stress. Complications can include urinary tract infections.

Enuresis is a repeated inability to control urination. Use of the term is usually limited to describing people old enough to be expected to exercise such control. Involuntary urination is also known as urinary incontinence. The term "enuresis" comes from the Ancient Greek: ἐνούρησις, romanized: enoúrēsis.

Stress incontinence, also known as stress urinary incontinence (SUI) or effort incontinence is a form of urinary incontinence. It is due to inadequate closure of the bladder outlet by the urethral sphincter.

Propantheline bromide (INN) is an antimuscarinic medication used for the treatment of excessive sweating (hyperhidrosis), cramps or spasms of the stomach, intestines (gut), or bladder, and involuntary urination (enuresis). It can also be used to control the symptoms of irritable bowel syndrome (IBS) and similar conditions. This medication can also be used for patients who experience intense gastrointestinal symptoms while tapering off of tricyclic antidepressants.

Solifenacin, sold as the brand name Vesicare among others, is a medicine used to treat overactive bladder and neurogenic detrusor overactivity (NDO). It may help with incontinence, urinary frequency, and urinary urgency.
Diurnal enuresis is daytime wetting. Nocturnal enuresis is nighttime wetting. Enuresis is defined as the involuntary voiding of urine beyond the age of anticipated control. Both of these conditions can occur at the same time, although many children with nighttime wetting will not have wetting during the day. Children with daytime wetting may have frequent urination, have urgent urination or dribble after urinating.

Bladder sphincter dyssynergia is a consequence of a neurological pathology such as spinal injury or multiple sclerosis which disrupts central nervous system regulation of the micturition (urination) reflex resulting in dyscoordination of the detrusor muscles of the bladder and the male or female external urethral sphincter muscles. In normal lower urinary tract function, these two separate muscle structures act in synergistic coordination. But in this neurogenic disorder, the urethral sphincter muscle, instead of relaxing completely during voiding, dyssynergically contracts causing the flow to be interrupted and the bladder pressure to rise.
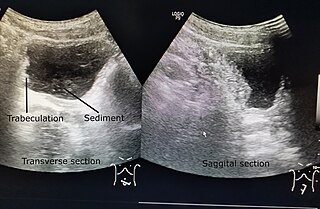
Neurogenic bladder dysfunction, often called by the shortened term neurogenic bladder, refers to urinary bladder problems due to disease or injury of the central nervous system or peripheral nerves involved in the control of urination. There are multiple types of neurogenic bladder depending on the underlying cause and the symptoms. Symptoms include overactive bladder, urinary urgency, frequency, incontinence or difficulty passing urine. A range of diseases or conditions can cause neurogenic bladder including spinal cord injury, multiple sclerosis, stroke, brain injury, spina bifida, peripheral nerve damage, Parkinson's disease, multiple system atrophy or other neurodegenerative diseases. Neurogenic bladder can be diagnosed through a history and physical as well as imaging and more specialized testing. In addition to symptomatic treatment, treatment depends on the nature of the underlying disease and can be managed with behavioral changes, medications, surgeries, or other procedures. The symptoms of neurogenic bladder, especially incontinence, can severely degrade a person's quality of life.

The detrusor muscle, also detrusor urinae muscle, muscularis propria of the urinary bladder and muscularis propria, is smooth muscle found in the wall of the bladder. The detrusor muscle remains relaxed to allow the bladder to store urine, and contracts during urination to release urine. Related are the urethral sphincter muscles which envelop the urethra to control the flow of urine when they contract.

Overactive bladder (OAB) is a common condition where there is a frequent feeling of needing to urinate to a degree that it negatively affects a person's life. The frequent need to urinate may occur during the day, at night, or both. Loss of bladder control may occur with this condition. This condition is also sometimes characterized by a sudden and involuntary contraction of the bladder muscles, in response to excitement or anticipation. This in turn leads to a frequent and urgent need to urinate.

The urethral sphincters are two muscles used to control the exit of urine in the urinary bladder through the urethra. The two muscles are either the male or female external urethral sphincter and the internal urethral sphincter. When either of these muscles contracts, the urethra is sealed shut.

The internal urethral sphincter is a urethral sphincter muscle which constricts the internal urethral orifice. It is located at the junction of the urethra with the urinary bladder and is continuous with the detrusor muscle, but anatomically and functionally fully independent from it. It is composed of smooth muscle, so it is under the control of the autonomic nervous system, specifically the sympathetic nervous system.
Sacral nerve stimulation, also termed sacral neuromodulation, is a type of medical electrical stimulation therapy.
Urologic diseases or conditions include urinary tract infections, kidney stones, bladder control problems, and prostate problems, among others. Some urologic conditions do not affect a person for that long and some are lifetime conditions. Kidney diseases are normally investigated and treated by nephrologists, while the specialty of urology deals with problems in the other organs. Gynecologists may deal with problems of incontinence in women.

Urodynamic testing or urodynamics is a study that assesses how the bladder and urethra are performing their job of storing and releasing urine. Urodynamic tests can help explain symptoms such as:

Overflow incontinence is a concept of urinary incontinence, characterized by the involuntary release of urine from an overfull urinary bladder, often in the absence of any urge to urinate. This condition occurs in people who have a blockage of the bladder outlet, or when the muscle that expels urine from the bladder is too weak to empty the bladder normally. Overflow incontinence may also be a side effect of certain medications.
A urethral bulking injection is a gynecological procedure and medical treatment used to treat involuntary leakage of urine: urinary incontinence in women. Injectional materials are used to control stress incontinence. Bulking agents are injected into the mucosa surrounding the bladder neck and proximal urethra. This reduces the diameter of the urethra and creates resistance to urine leakage. After the procedure, the pressure forcing the urine from the bladder through the urethra is resisted by the addition of the bulking agent in the tissue surrounding the proximal urethra. Most of the time this procedure prevents urinary stress incontinence in women.
Karl-Erik Andersson is a Swedish pharmacologist and academic. He is a professor emeritus in the Institute for Regenerative Medicine at Wake Forest University School of Medicine and in the Division of Clinical Chemistry and Pharmacology at Lund University.
References
- 1 2 Glahn, B. E. (1979). "Giggle Incontinence (Enuresis Risoria). A Study and an Aetiological Hypothesis". British Journal of Urology. 51 (5): 363–366. doi:10.1111/j.1464-410X.1979.tb02887.x. PMID 533593.
- 1 2 Cooper, Christopher S (2010). "Voiding Dysfunction Clinical Presentation". Medscape . Retrieved June 3, 2011.
- 1 2 3 4 5 Carlin & Leong (2002). Female Pelvic Health and Reconstructive Surgery. Informa Healthcare. ISBN 978-0-8247-0822-1 . Retrieved May 30, 2011.
- ↑ Liedl et al & Viktrup; et al. (2004–2005). "Urinary Incontinence: Causes and Diagnostic Work-Up". Urology-Textbook.com. Retrieved June 3, 2011.
- ↑ Chandra, M; Saharia, R; Shi, Q; Hill, V (2002). "Giggle incontinence in children: a manifestation of detrusor instability". The Journal of Urology. 168 (5): 2184–7, discussion 2187. doi:10.1016/s0022-5347(05)64350-9. PMID 12394756.
- ↑ Abrams, Paul (2006). "Giggle Incontinence". Urodynamics. Birkhäuser. p. 129. ISBN 978-1-85233-924-1.
- 1 2 Kher, Schnaper & Makker (2006). Clinical pediatric nephrology. Informa Healthcare. p. 520. ISBN 978-1-84184-447-3 . Retrieved May 30, 2011.
- 1 2 "Developing - School - Giggle Incontinence". ParentsCanada.com. Archived from the original on October 5, 2011. Retrieved May 30, 2011.
- 1 2 Berry, Amanda K.; Zderic, Stephen; Carr, Michael (2009). "Methylphenidate for Giggle Incontinence". The Journal of Urology. 182 (4): 2028–32. doi:10.1016/j.juro.2009.04.085. PMID 19695642.