Vascular dementia is dementia caused by a series of strokes. Restricted blood flow due to strokes reduces oxygen and glucose delivery to the brain, causing cell injury and neurological deficits in the affected region. Subtypes of vascular dementia include subcortical vascular dementia, multi-infarct dementia, stroke-related dementia, and mixed dementia.
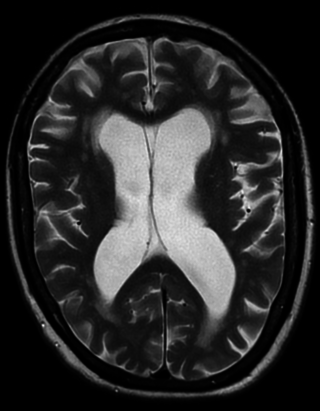
Porencephaly is an extremely rare cephalic disorder involving encephalomalacia. It is a neurological disorder of the central nervous system characterized by cysts or cavities within the cerebral hemisphere. Porencephaly was termed by Heschl in 1859 to describe a cavity in the human brain. Derived from Greek roots, the word porencephaly means 'holes in the brain'. The cysts and cavities are more likely to be the result of destructive (encephaloclastic) cause, but can also be from abnormal development (malformative), direct damage, inflammation, or hemorrhage. The cysts and cavities cause a wide range of physiological, physical, and neurological symptoms. Depending on the patient, this disorder may cause only minor neurological problems, without any disruption of intelligence, while others may be severely disabled or die before the second decade of their lives. However, this disorder is far more common within infants, and porencephaly can occur both before or after birth.

Cerebrovascular disease includes a variety of medical conditions that affect the blood vessels of the brain and the cerebral circulation. Arteries supplying oxygen and nutrients to the brain are often damaged or deformed in these disorders. The most common presentation of cerebrovascular disease is an ischemic stroke or mini-stroke and sometimes a hemorrhagic stroke. Hypertension is the most important contributing risk factor for stroke and cerebrovascular diseases as it can change the structure of blood vessels and result in atherosclerosis. Atherosclerosis narrows blood vessels in the brain, resulting in decreased cerebral perfusion. Other risk factors that contribute to stroke include smoking and diabetes. Narrowed cerebral arteries can lead to ischemic stroke, but continually elevated blood pressure can also cause tearing of vessels, leading to a hemorrhagic stroke.

Intracranial hemorrhage (ICH), also known as intracranial bleed, is bleeding within the skull. Subtypes are intracerebral bleeds, subarachnoid bleeds, epidural bleeds, and subdural bleeds.
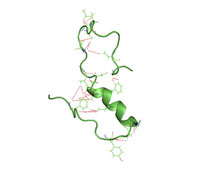
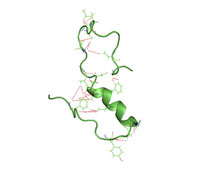
Amyloid beta denotes peptides of 36–43 amino acids that are the main component of the amyloid plaques found in the brains of people with Alzheimer's disease. The peptides derive from the amyloid-beta precursor protein (APP), which is cleaved by beta secretase and gamma secretase to yield Aβ in a cholesterol-dependent process and substrate presentation. Aβ molecules can aggregate to form flexible soluble oligomers which may exist in several forms. It is now believed that certain misfolded oligomers can induce other Aβ molecules to also take the misfolded oligomeric form, leading to a chain reaction akin to a prion infection. The oligomers are toxic to nerve cells. The other protein implicated in Alzheimer's disease, tau protein, also forms such prion-like misfolded oligomers, and there is some evidence that misfolded Aβ can induce tau to misfold.

Cerebral amyloid angiopathy (CAA) is a form of angiopathy in which amyloid beta peptide deposits in the walls of small to medium blood vessels of the central nervous system and meninges. The term congophilic is sometimes used because the presence of the abnormal aggregations of amyloid can be demonstrated by microscopic examination of brain tissue after staining with Congo red. The amyloid material is only found in the brain and as such the disease is not related to other forms of amyloidosis.

A perivascular space, also known as a Virchow–Robin space, is a fluid-filled space surrounding certain blood vessels in several organs, including the brain, potentially having an immunological function, but more broadly a dispersive role for neural and blood-derived messengers. The brain pia mater is reflected from the surface of the brain onto the surface of blood vessels in the subarachnoid space. In the brain, perivascular cuffs are regions of leukocyte aggregation in the perivascular spaces, usually found in patients with viral encephalitis.

Intracerebral hemorrhage (ICH), also known as hemorrhagic stroke, is a sudden bleeding into the tissues of the brain, into its ventricles, or into both. An ICH is a type of bleeding within the skull and one kind of stroke. Symptoms can vary dramatically depending on the severity, acuity, and location (anatomically) but can include headache, one-sided weakness, numbness, tingling, or paralysis, speech problems, vision or hearing problems, memory loss, attention problems, coordination problems, balance problems, dizziness or lightheadedness or vertigo, nausea/vomiting, seizures, decreased level of consciousness or total loss of consciousness, neck stiffness, and fever.

Intraparenchymal hemorrhage (IPH) is one form of intracerebral bleeding in which there is bleeding within brain parenchyma. The other form is intraventricular hemorrhage (IVH).

Cystatin C or cystatin 3, a protein encoded by the CST3 gene, is mainly used as a biomarker of kidney function. Recently, it has been studied for its role in predicting new-onset or deteriorating cardiovascular disease. It also seems to play a role in brain disorders involving amyloid, such as Alzheimer's disease. In humans, all cells with a nucleus produce cystatin C as a chain of 120 amino acids. It is found in virtually all tissues and body fluids. It is a potent inhibitor of lysosomal proteinases and probably one of the most important extracellular inhibitors of cysteine proteases. Cystatin C belongs to the type 2 cystatin gene family.

Cystatin-SA is a protein that in humans is encoded by the CST2 gene.

Alzheimer's disease (AD) is a neurodegenerative disease that usually starts slowly and progressively worsens, and is the cause of 60–70% of cases of dementia. The most common early symptom is difficulty in remembering recent events. As the disease advances, symptoms can include problems with language, disorientation, mood swings, loss of motivation, self-neglect, and behavioral issues. As a person's condition declines, they often withdraw from family and society. Gradually, bodily functions are lost, ultimately leading to death. Although the speed of progression can vary, the average life expectancy following diagnosis is three to twelve years.
Early-onset Alzheimer's disease (EOAD), also called younger-onset Alzheimer's disease (YOAD), is Alzheimer's disease diagnosed before the age of 65. It is an uncommon form of Alzheimer's, accounting for only 5–10% of all Alzheimer's cases. About 60% have a positive family history of Alzheimer's and 13% of them are inherited in an autosomal dominant manner. Most cases of early-onset Alzheimer's share the same traits as the "late-onset" form and are not caused by known genetic mutations. Little is understood about how it starts.
Reversible cerebral vasoconstriction syndrome is a disease characterized by a weeks-long course of thunderclap headaches, sometimes focal neurologic signs, and occasionally seizures. Symptoms are thought to arise from transient abnormalities in the blood vessels of the brain. In some cases, it may be associated with childbirth, vasoactive or illicit drug use, or complications of pregnancy. If it occurs after delivery it may be referred to as postpartum cerebral angiopathy.

Hereditary diffuse leukoencephalopathy with spheroids (HDLS) is a rare adult onset autosomal dominant disorder characterized by cerebral white matter degeneration with demyelination and axonal spheroids leading to progressive cognitive and motor dysfunction. Spheroids are axonal swellings with discontinuous or absence of myelin sheaths. It is believed that the disease arises from primary microglial dysfunction that leads to secondary disruption of axonal integrity, neuroaxonal damage, and focal axonal spheroids leading to demyelination. Spheroids in HDLS resemble to some extent those produced by shear stress in a closed head injury with damage to axons, causing them to swell due to blockage of axoplasmic transport. In addition to trauma, axonal spheroids can be found in aged brain, stroke, and in other degenerative diseases. In HDLS, it is uncertain whether demyelination occurs prior to the axonal spheroids or what triggers neurodegeneration after apparently normal brain and white matter development, although genetic deficits suggest that demyelination and axonal pathology may be secondary to microglial dysfunction. The clinical syndrome in patients with HDLS is not specific and it can be mistaken for Alzheimer's disease, frontotemporal dementia, atypical Parkinsonism, multiple sclerosis, or corticobasal degeneration.

Cerebral atherosclerosis is a type of atherosclerosis where build-up of plaque in the blood vessels of the brain occurs. Some of the main components of the plaques are connective tissue, extracellular matrix, including collagen, proteoglycans, fibronectin, and elastic fibers; crystalline cholesterol, cholesteryl esters, and phospholipids; cells such as monocyte derived macrophages, T-lymphocytes, and smooth muscle cells. The plaque that builds up can lead to further complications such as stroke, as the plaque disrupts blood flow within the intracranial arterioles. This causes the downstream sections of the brain that would normally be supplied by the blocked artery to suffer from ischemia. Diagnosis of the disease is normally done through imaging technology such as angiograms or magnetic resonance imaging. The risk of cerebral atherosclerosis and its associated diseases appears to increase with increasing age; however there are numerous factors that can be controlled in attempt to lessen risk.

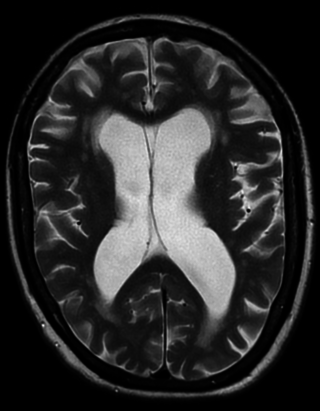
Amyloid-related imaging abnormalities (ARIA) are abnormal differences seen in magnetic resonance imaging of the brain in patients with Alzheimer's disease. ARIA is associated with anti-amyloid drugs, particularly human monoclonal antibodies such as aducanumab. There are two types of ARIA: ARIA-E and ARIA-H. The phenomenon was first seen in trials of bapineuzumab.
Familial Danish Dementia is an extremely rare, neurodegenerative disease characterized by progressive cataracts, loss of hearing, cerebellar ataxia, paranoid psychosis, and dementia. Neuropathological hallmarks include extensive atrophy of all areas of the brain, chronic diffuse encephalopathy, and the presence of exceedingly thin and nearly totally demyelinated cranial nerves.
Anders Grubb is a Swedish chemist, physician, and academic. He is currently a Senior Professor of Clinical Chemistry at Lund University.
The Boston criteria version 2.0 is a set of guidelines designed to diagnose cerebral amyloid angiopathy (CAA), a disease that affects small blood vessels in the brain, particularly those in the cortex and leptomeninges. Although the gold standard for diagnosis is histopathological examination, the Boston criteria provide clinicians with a probabilistic approach for diagnosis largely based on imaging characteristics.