A testicle or testis is the male reproductive gland or gonad in all bilaterians, including humans. It is homologous to the female ovary. The functions of the testes are to produce both sperm and androgens, primarily testosterone. Testosterone release is controlled by the anterior pituitary luteinizing hormone, whereas sperm production is controlled both by the anterior pituitary follicle-stimulating hormone and gonadal testosterone.

Testicular torsion occurs when the spermatic cord twists, cutting off the blood supply to the testicle. The most common symptom in children is sudden, severe testicular pain. The testicle may be higher than usual in the scrotum and vomiting may occur. In newborns, pain is often absent and instead the scrotum may become discolored or the testicle may disappear from its usual place.

Testicular cancer is cancer that develops in the testicles, a part of the male reproductive system. Symptoms may include a lump in the testicle or swelling or pain in the scrotum. Treatment may result in infertility.

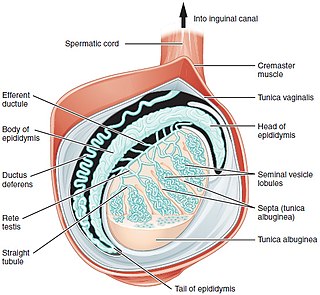
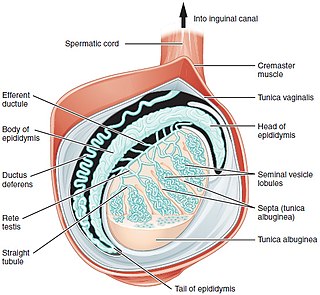
The spermatic cord is the cord-like structure in males formed by the vas deferens and surrounding tissue that runs from the deep inguinal ring down to each testicle. Its serosal covering, the tunica vaginalis, is an extension of the peritoneum that passes through the transversalis fascia. Each testicle develops in the lower thoracic and upper lumbar region and migrates into the scrotum. During its descent it carries along with it the vas deferens, its vessels, nerves etc. There is one on each side.

The inguinal canal is a passage in the anterior abdominal wall on each side of the body which in males convey the spermatic cords and in females the round ligament of the uterus. The inguinal canals are larger and more prominent in males.

A hydrocele testis is an accumulation of clear fluid within the cavum vaginale, the potential space between the layers of the tunica vaginalis of the testicle. It is the most common form of hydrocele and is often referred to simply as a "hydrocele". A primary hydrocele testis causes a painless enlargement in the scrotum on the affected side and is thought to be due to the defective absorption of fluid secreted between the two layers of the tunica vaginalis. A secondary hydrocele is secondary to either inflammation or a neoplasm in the testis.
Orchitis is inflammation of the testes. It can also involve swelling, pains and frequent infection, particularly of the epididymis, as in epididymitis. The term is from the Ancient Greek ὄρχις meaning "testicle"; same root as orchid.

Orchiopexy is a surgery to move and/or permanently fix a testicle into the scrotum. While orchiopexy typically describes the operation to surgically correct an undescended testicle, it is also used to resolve testicular torsion.
An inguinal hernia or groin hernia, is a hernia (protrusion) of abdominal cavity contents through the inguinal canal. Symptoms, which may include pain or discomfort especially with or following coughing, exercise, or bowel movements, are absent in about a third of patients. Symptoms often get worse throughout the day and improve when lying down. A bulging area may occur that becomes larger when bearing down. Inguinal hernias occur more often on the right than left side. The main concern is strangulation, where the blood supply to part of the intestine is blocked. This usually produces severe pain and tenderness of the area.

Spermatocele is a fluid-filled cyst that develops in the epididymis. The fluid is usually a clear or milky white color and may contain sperm. Spermatoceles are typically filled with spermatozoa and they can vary in size from several millimeters to many centimeters. Small spermatoceles are relatively common, occurring in an estimated 30 percent of males. They are generally not painful. However, some people may experience discomfort such as a dull pain in the scrotum from larger spermatoceles. They are not cancerous, nor do they cause an increased risk of testicular cancer. Additionally, unlike varicoceles, they do not reduce fertility.

A hematocele is a collections of blood in a body cavity or potential space. The term most commonly refers to the collection of blood in the tunica vaginalis around the testes, known as a scrotal hematocele. Hematoceles can also occur in the abdominal cavity and other body cavities. Hematoceles are rare, making them harder to diagnose and treat. They are very common especially as slowly growing masses in the scrotum usually in men older than 50 years.
Transillumination is the technique of sample illumination by transmission of light through the sample. Transillumination is used in a variety of methods of imaging.
Inguinal orchiectomy is a specific method of orchiectomy whereby one or both testicles and the full spermatic cord are surgically removed through an incision in the lower lateral abdomen. The procedure is generally performed by a urologist, typically if testicular cancer is suspected. Often it is performed as same-day surgery, with the patient returning home within hours of the procedure. Some patients elect to have a prosthetic testicle inserted into their scrotum. Depending on whether or not a prosthetic testicle is put in place of the original one, operating times run on average from three to six hours.
The canal of Nuck, first described by Anton Nuck in 1691, is an abnormal patent (open) pouch of peritoneum extending into the labia majora of women. It is analogous to a patent processus vaginalis in males. In rare cases, it may give rise to a cyst or a hydrocele in women and has potential to develop into an indirect inguinal hernia. The pouch accompanies the gubernaculum during development of the urinary and reproductive organs, more specifically during the descent of the ovaries, and normally obliterates.
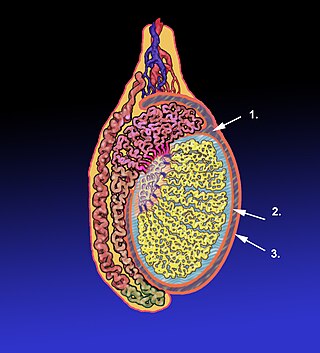
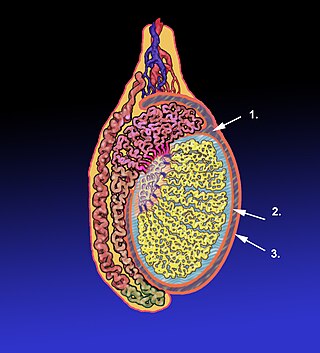
The tunica vaginalis is a pouch of serous membrane within the scrotum that lines the testis and epididymis, and the inner surface of the scrotum. It is the outermost of the three layers that constitute the capsule of the testis, with the tunica albuginea of penis situated beneath it.

The vaginal process is an embryonic developmental outpouching of the parietal peritoneum. It is present from around the 12th week of gestation, and commences as a peritoneal outpouching.
The development of the gonads is part of the prenatal development of the reproductive system and ultimately forms the testes in males and the ovaries in females. The gonads initially develop from the mesothelial layer of the peritoneum.

The scrotum or scrotal sac is an anatomical male reproductive structure located at the base of the penis that consists of a suspended dual-chambered sac of skin and smooth muscle. It is present in most terrestrial male mammals. The scrotum contains the external spermatic fascia, testicles, epididymis, and ductus deferens. It is a distention of the perineum and carries some abdominal tissues into its cavity including the testicular artery, testicular vein, and pampiniform plexus. The perineal raphe is a small, vertical, slightly raised ridge of scrotal skin under which is found the scrotal septum. It appears as a thin longitudinal line that runs front to back over the entire scrotum. In humans and some other mammals, the scrotum becomes covered with pubic hair at puberty. The scrotum will usually tighten during penile erection and when exposed to cold temperatures. One testis is typically lower than the other to avoid compression in the event of an impact.

Scrotalultrasound is a medical ultrasound examination of the scrotum. It is used in the evaluation of testicular pain, and can help identify solid masses.
Male genital examination is a physical examination of the genital in males to detect ailments and to assess sexual development and is normally included in an annual physical examination. The examination includes checking the penis, scrotum, and urethral meatus. A comprehensive assessment of the male genitals assesses the pubic hair based on Sexual Maturity Rating and the size of the testicles and penis. The exam is conducted to detect various ailments, measure sexual development, or verify a person's age and biological sex. The genitourinary system can also be assessed as part of the male genital examination. During a genital examination, the doctor can detect any of the following: structural abnormalities, urethral opening abnormalities, problems related to uncircumcision, lumps, tumors, redness, excoriation, edema, lesions, swelling, cancer, hair-related issues and many others. In some instances where a physical examination of the male genitals is not sufficient to diagnose an individual than an internal genital examination using imaging or ultrasounds will be needed for further evaluation.