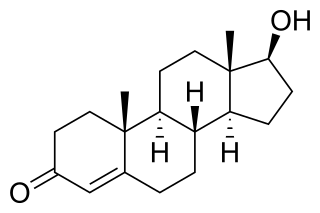
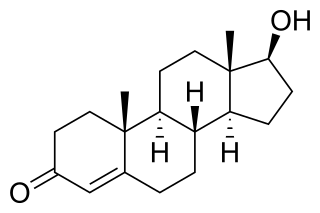
Progesterone (P4) is an endogenous steroid and progestogen sex hormone involved in the menstrual cycle, pregnancy, and embryogenesis of humans and other species. It belongs to a group of steroid hormones called the progestogens and is the major progestogen in the body. Progesterone has a variety of important functions in the body. It is also a crucial metabolic intermediate in the production of other endogenous steroids, including the sex hormones and the corticosteroids, and plays an important role in brain function as a neurosteroid.

A progestogen, also referred to as a progestagen, gestagen, or gestogen, is a type of medication which produces effects similar to those of the natural female sex hormone progesterone in the body. A progestin is a synthetic progestogen. Progestogens are used most commonly in hormonal birth control and menopausal hormone therapy. They can also be used in the treatment of gynecological conditions, to support fertility and pregnancy, to lower sex hormone levels for various purposes, and for other indications. Progestogens are used alone or in combination with estrogens. They are available in a wide variety of formulations and for use by many different routes of administration. Examples of progestogens include natural or bioidentical progesterone as well as progestins such as medroxyprogesterone acetate and norethisterone.

Levonorgestrel is a hormonal medication which is used in a number of birth control methods. It is combined with an estrogen to make combination birth control pills. As an emergency birth control, sold under the brand names Plan B One-Step and Julie, among others, it is useful within 72 hours of unprotected sex. The more time that has passed since sex, the less effective the medication becomes, and it does not work after pregnancy (implantation) has occurred. Levonorgestrel works by preventing ovulation or fertilization from occurring. It decreases the chances of pregnancy by 57–93%. In an intrauterine device (IUD), such as Mirena among others, it is effective for the long-term prevention of pregnancy. A levonorgestrel-releasing implant is also available in some countries.
Hot flashes, also known as hot flushes, are a form of flushing, often caused by the changing hormone levels that are characteristic of menopause. They are typically experienced as a feeling of intense heat with sweating and rapid heartbeat, and may typically last from two to 30 minutes for each occurrence.
Bioidentical hormone replacement therapy (BHRT), also known as bioidentical hormone therapy (BHT) or natural hormone therapy, is the use of hormones that are identical on a molecular level with endogenous hormones in hormone replacement therapy. It may also be combined with blood and saliva testing of hormone levels, and the use of pharmacy compounding to obtain hormones in an effort to reach a targeted level of hormones in the body. A number of claims by some proponents of BHT have not been confirmed through scientific testing. Specific hormones used in BHT include estrone, estradiol, progesterone, testosterone, dehydroepiandrosterone (DHEA), and estriol.

Drospirenone is a progestin and antiandrogen medication which is used in birth control pills to prevent pregnancy and in menopausal hormone therapy, among other uses. It is available both alone under the brand name Slynd and in combination with an estrogen under the brand name Yasmin among others. The medication is an analog of the drug spironolactone. Drospirenone is taken by mouth.

Norelgestromin, or norelgestromine, sold under the brand names Evra and Ortho Evra among others, is a progestin medication which is used as a method of birth control for women. The medication is available in combination with an estrogen and is not available alone. It is used as a patch that is applied to the skin.
Hormone replacement therapy (HRT), also known as menopausal hormone therapy or postmenopausal hormone therapy, is a form of hormone therapy used to treat symptoms associated with female menopause. Effects of menopause can include symptoms such as hot flashes, accelerated skin aging, vaginal dryness, decreased muscle mass, and complications such as osteoporosis, sexual dysfunction, and vaginal atrophy. They are mostly caused by low levels of female sex hormones that occur during menopause.

Trimegestone, sold under the brand names Ondeva and Totelle among others, is a progestin medication which is used in menopausal hormone therapy and in the prevention of postmenopausal osteoporosis. It was also under development for use in birth control pills to prevent pregnancy, but ultimately was not marketed for this purpose. The medication is available alone or in combination with an estrogen. It is taken by mouth.

Hydroxyprogesterone heptanoate (OHPH), also known as hydroxyprogesterone enanthate (OHPE) and sold under the brand names H.O.P., Lutogil A.P., and Lutogyl A.P. among others, is a progestin medication used for progestogenic indications. It has been formulated both alone and in together with estrogens, androgens/anabolic steroids, and other progestogens in several combination preparations. OHPH is given by injection into muscle at regular intervals.

Conjugated estrogens (CEs), or conjugated equine estrogens (CEEs), sold under the brand name Premarin among others, is an estrogen medication which is used in menopausal hormone therapy and for various other indications. It is a mixture of the sodium salts of estrogen conjugates found in horses, such as estrone sulfate and equilin sulfate. CEEs are available in the form of both natural preparations manufactured from the urine of pregnant mares and fully synthetic replications of the natural preparations. They are formulated both alone and in combination with progestins such as medroxyprogesterone acetate. CEEs are usually taken by mouth, but can also be given by application to the skin or vagina as a cream or by injection into a blood vessel or muscle.

Estradiol/progesterone (E2/P4), sold under the brand name Bijuva among others, is a combined estrogen and progestogen medication which is used in the treatment of menopausal symptoms in postmenopausal women. It contains estradiol, an estrogen, and progesterone, a progestogen, and is available in both oral and intramuscular formulations. E2/P4 differs from other estrogen–progestogen formulations in that the sex-hormonal agents used are bioidentical.

Estradiol (E2) is a medication and naturally occurring steroid hormone. It is an estrogen and is used mainly in menopausal hormone therapy and to treat low sex hormone levels in women. It is also used in hormonal birth control for women, in feminizing hormone therapy for transgender women and some non-binary individuals, and in the treatment of hormone-sensitive cancers like prostate cancer in men and breast cancer in women, among other uses. Estradiol can be taken by mouth, held and dissolved under the tongue, as a gel or patch that is applied to the skin, in through the vagina, by injection into muscle or fat, or through the use of an implant that is placed into fat, among other routes.

Progesterone (P4), sold under the brand name Prometrium among others, is a medication and naturally occurring steroid hormone. It is a progestogen and is used in combination with estrogens mainly in hormone therapy for menopausal symptoms and low sex hormone levels in women. It is also used in women to support pregnancy and fertility and to treat gynecological disorders. Progesterone can be taken by mouth, vaginally, and by injection into muscle or fat, among other routes. A progesterone vaginal ring and progesterone intrauterine device used for birth control also exist in some areas of the world.

Prasterone enanthate, also known as dehydroepiandrosterone enanthate (DHEA-E) and sold in combination with estradiol valerate under the brand name Gynodian Depot among others, is a weak androgen, estrogen, and neurosteroid medication which is used as a component of menopausal hormone therapy to treat menopausal symptoms in women. It is available only as an injectable preparation in combination with estradiol valerate. The medication is given by injection into muscle typically once every 4 weeks.

The pharmacology of estradiol, an estrogen medication and naturally occurring steroid hormone, concerns its pharmacodynamics, pharmacokinetics, and various routes of administration.

The pharmacokinetics of progesterone, concerns the pharmacodynamics, pharmacokinetics, and various routes of administration of progesterone.
The pharmacology of testosterone, an androgen and anabolic steroid (AAS) medication and naturally occurring steroid hormone, concerns its pharmacodynamics, pharmacokinetics, and various routes of administration.
The Menopause, Estrogen and Venous Events (MEVE) study was a retrospective observational study of menopausal hormone therapy and venous thromboembolism (VTE) in postmenopausal women with a previous history of VTE. It found that transdermal estradiol was not associated with increased risk of VTE whereas oral estrogens were associated with a large increase in risk. The mean dose of transdermal estradiol in the study was 50 μg/day, although data on dose were missing for around 50% of women. Similarly, a small study found that transdermal estradiol did not influence coagulation in women with prior VTE. These findings are similar to studies in menopausal women without prior history of VTE which have found that transdermal estradiol has minimal influence on coagulation and is not associated with increased risk of VTE at doses of up to 100 μg/day. Menopausal hormone therapy guidelines have cited the MEVE study and recommended use of transdermal estradiol over oral estrogens in women at high risk for VTE. However, randomized controlled trials (RCTs) are still needed to definitively confirm findings that transdermal estradiol is safer than oral estrogens in terms of VTE risk.