Gastroenterology is the branch of medicine focused on the digestive system and its disorders. The digestive system consists of the gastrointestinal tract, sometimes referred to as the GI tract, which includes the esophagus, stomach, small intestine and large intestine as well as the accessory organs of digestion which include the pancreas, gallbladder, and liver.

Peptic ulcer disease is a break in the inner lining of the stomach, the first part of the small intestine, or sometimes the lower esophagus. An ulcer in the stomach is called a gastric ulcer, while one in the first part of the intestines is a duodenal ulcer. The most common symptoms of a duodenal ulcer are waking at night with upper abdominal pain, and upper abdominal pain that improves with eating. With a gastric ulcer, the pain may worsen with eating. The pain is often described as a burning or dull ache. Other symptoms include belching, vomiting, weight loss, or poor appetite. About a third of older people with peptic ulcers have no symptoms. Complications may include bleeding, perforation, and blockage of the stomach. Bleeding occurs in as many as 15% of cases.

Esophageal achalasia, often referred to simply as achalasia, is a failure of smooth muscle fibers to relax, which can cause the lower esophageal sphincter to remain closed. Without a modifier, "achalasia" usually refers to achalasia of the esophagus. Achalasia can happen at various points along the gastrointestinal tract; achalasia of the rectum, for instance, may occur in Hirschsprung's disease. The lower esophageal sphincter is a muscle between the esophagus and stomach that opens when food comes in. It closes to avoid stomach acids from coming back up. A fully understood cause to the disease is unknown, as are factors that increase the risk of its appearance. Suggestions of a genetically transmittable form of achalasia exist, but this is neither fully understood, nor agreed upon.
Heartburn, also known as pyrosis, cardialgia or acid indigestion, is a burning sensation in the central chest or upper central abdomen. Heartburn is usually due to regurgitation of gastric acid into the esophagus. It is the major symptom of gastroesophageal reflux disease (GERD).

Gastroesophageal reflux disease (GERD) or gastro-oesophageal reflux disease (GORD) is a chronic upper gastrointestinal disease in which stomach content persistently and regularly flows up into the esophagus, resulting in symptoms and/or complications. Symptoms include dental corrosion, dysphagia, heartburn, odynophagia, regurgitation, non-cardiac chest pain, extraesophageal symptoms such as chronic cough, hoarseness, reflux-induced laryngitis, or asthma. In the long term, and when not treated, complications such as esophagitis, esophageal stricture, and Barrett's esophagus may arise.

Barrett's esophagus is a condition in which there is an abnormal (metaplastic) change in the mucosal cells lining the lower portion of the esophagus, from stratified squamous epithelium to simple columnar epithelium with interspersed goblet cells that are normally present only in the small intestine and large intestine. This change is considered to be a premalignant condition because of its potential to further transition to esophageal adenocarcinoma, an often-deadly cancer.

Esophagitis, also spelled oesophagitis, is a disease characterized by inflammation of the esophagus. The esophagus is a tube composed of a mucosal lining, and longitudinal and circular smooth muscle fibers. It connects the pharynx to the stomach; swallowed food and liquids normally pass through it.
Coffee ground vomitus refers to a particular appearance of vomit. Within organic heme molecules of red blood cells is the element iron, which oxidizes following exposure to gastric acid. This reaction causes the vomitus to look like ground coffee.

Mallory–Weiss syndrome is a condition where high intra-abdominal pressures causes laceration and bleeding of the mucosa called Mallory-Weiss tears. Additionally, Mallory–Weiss syndrome is one of the most common causes of acute upper gastrointestinal bleeding, counting of around 1-15% of all cases in adults and less than 5% in children. It has been found that tears are up to 2 to 4 times more prevalent in men than women. The tears can cause upper gastrointestinal bleeding and predominantly occur where the esophagus meets the stomach. However, the tears can happen anywhere from the middle of the esophagus to the cardia of the stomach. Mallory–Weiss syndrome is often caused by constant vomiting and retching from alcoholism or bulimia. Gastroesophageal reflux disease (GERD) is another risk factor that is often linked with Mallory–Weiss syndrome. However, not every individual with Mallory–Weiss syndrome will have these risk factors. Individuals with Mallory–Weiss syndrome will have hematemesis, however the symptoms can vary.

Plummer–Vinson syndrome is a rare disease characterized by dysphagia, iron-deficiency anemia, glossitis, cheilosis, and esophageal webs. Treatment with iron supplementation and mechanical widening of the esophagus generally leads to excellent outcomes.

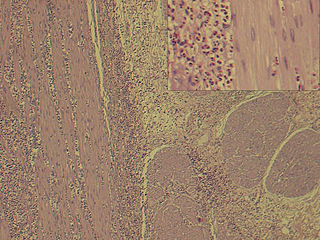
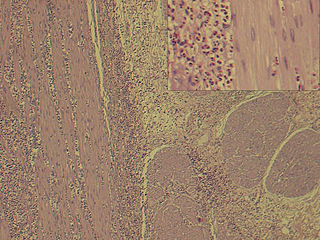
Microscopic colitis refers to two related medical conditions which cause diarrhea: collagenous colitis and lymphocytic colitis. Both conditions are characterized by the presence of chronic non-bloody watery diarrhea, normal appearances on colonoscopy and characteristic histopathology findings of inflammatory cells.

Eosinophilic esophagitis (EoE) is an allergic inflammatory condition of the esophagus that involves eosinophils, a type of white blood cell. In healthy individuals, the esophagus is typically devoid of eosinophils. In EoE, eosinophils migrate to the esophagus in large numbers. When a trigger food is eaten, the eosinophils contribute to tissue damage and inflammation. Symptoms include swallowing difficulty, food impaction, vomiting, and heartburn.
Esophageal dysphagia is a form of dysphagia where the underlying cause arises from the body of the esophagus, lower esophageal sphincter, or cardia of the stomach, usually due to mechanical causes or motility problems.
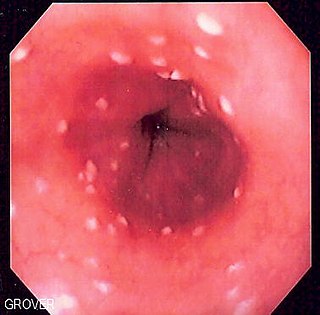
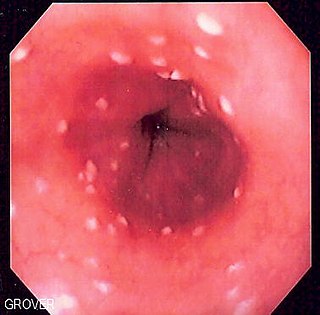
Esophageal candidiasis is an opportunistic infection of the esophagus by Candida albicans. The disease usually occurs in patients in immunocompromised states, including post-chemotherapy and in AIDS. However, it can also occur in patients with no predisposing risk factors, and is more likely to be asymptomatic in those patients. It is also known as candidal esophagitis or monilial esophagitis.
Eosinophilic gastroenteritis, also known as eosinophilic enteritis, is a rare and heterogeneous condition characterized by patchy or diffuse eosinophilic infiltration of gastrointestinal (GI) tissue, first described by Kaijser in 1937. Presentation may vary depending on location as well as depth and extent of bowel wall involvement and usually runs a chronic relapsing course. It can be classified into mucosal, muscular and serosal types based on the depth of involvement. Any part of the GI tract can be affected, and isolated biliary tract involvement has also been reported. The stomach is the organ most commonly affected, followed by the small intestine and the colon.

An esophageal food bolus obstruction is a medical emergency caused by the obstruction of the esophagus by an ingested foreign body.

Acute esophageal necrosis (AEN), black esophagus, or Gurvits syndrome is a rare esophageal disorder. AEN defines itself with dark pigmentation of the esophagus, found during an upper gastrointestinal endoscopy. Pigmentation is usually black friable mucosa. The disorder is extremely rare, as only 89 patients over a span of 40 years have received this diagnosis. Specific study of the disorder's mortality rate is mentioned at 31.8%, but new research suggests mortality rates vary from 30 to 50%. The exact triggering mechanism for this disorder is still unknown, but is likely multifactorial.

In gastroenterology, esophageal pH monitoring is the current gold standard for diagnosis of gastroesophageal reflux disease (GERD). It provides direct physiologic measurement of acid in the esophagus and is the most objective method to document reflux disease, assess the severity of the disease and monitor the response of the disease to medical or surgical treatment. It can also be used in diagnosing laryngopharyngeal reflux.

Herpes esophagitis is a viral infection of the esophagus caused by Herpes simplex virus (HSV).

Esophageal intramucosal pseudodiverticulosis (EIPD) is a rare condition wherein the esophagus wall develops numerous small outpouchings (pseudodiverticulae). Individuals with the condition typically develop difficulty swallowing. The outpouchings represent the ducts of the submucosal glands of the esophagus. It typically affects individuals in their sixth and seventh decades of life. While it is associated with certain chronic conditions, particularly alcoholism, diabetes and gastroesophageal reflux disease, the cause of the condition is unknown. Treatment involves medications to treat concomitant conditions such as reflux esophageal spasm, and dilation of strictures in the esophagus.