Related Research Articles
Post-traumatic stress disorder (PTSD) is a mental and behavioral disorder that develops from experiencing a traumatic event, such as sexual assault, warfare, traffic collisions, child abuse, domestic violence, or other threats on a person's life or well-being. Symptoms may include disturbing thoughts, feelings, or dreams related to the events, mental or physical distress to trauma-related cues, attempts to avoid trauma-related cues, alterations in the way a person thinks and feels, and an increase in the fight-or-flight response. These symptoms last for more than a month after the event. Young children are less likely to show distress, but instead may express their memories through play. A person with PTSD is at a higher risk of suicide and intentional self-harm.

Combat stress reaction (CSR) is acute behavioral disorganization as a direct result of the trauma of war. Also known as "combat fatigue", "battle fatigue", or "battle neurosis", it has some overlap with the diagnosis of acute stress reaction used in civilian psychiatry. It is historically linked to shell shock and can sometimes precurse post-traumatic stress disorder.

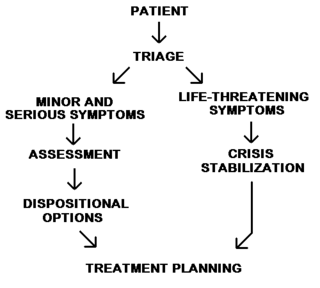
Emergency psychiatry is the clinical application of psychiatry in emergency settings. Conditions requiring psychiatric interventions may include attempted suicide, substance abuse, depression, psychosis, violence or other rapid changes in behavior. Psychiatric emergency services are rendered by professionals in the fields of medicine, nursing, psychology and social work. The demand for emergency psychiatric services has rapidly increased throughout the world since the 1960s, especially in urban areas. Care for patients in situations involving emergency psychiatry is complex.
Liaison psychiatry, also known as consultative psychiatry or consultation-liaison psychiatry, is the branch of psychiatry that specialises in the interface between general medicine/pediatrics and psychiatry, usually taking place in a hospital or medical setting. The role of the consultation-liaison psychiatrist is to see patients with comorbid medical conditions at the request of the treating medical or surgical consultant or team. Consultation-liaison psychiatry has areas of overlap with other disciplines including psychosomatic medicine, health psychology and neuropsychiatry.
Peer support occurs when people provide knowledge, experience, emotional, social or practical help to each other. It commonly refers to an initiative consisting of trained supporters, and can take a number of forms such as peer mentoring, reflective listening, or counseling. Peer support is also used to refer to initiatives where colleagues, members of self-help organizations and others meet, in person or online, as equals to give each other connection and support on a reciprocal basis.
Mental health in China is a growing issue. Experts have estimated that about 173 million people living in China are suffering from a mental disorder. The desire to seek treatment is largely hindered by China's strict social norms, as well as religious and cultural beliefs regarding personal reputation and social harmony.
Psychiatric and mental health nurses in the U.S. Army Nurse Corps employing groundbreaking protocols and treatments in psychiatric issues to address the unique challenges that our service men and women face, more commonly post-traumatic stress disorder and traumatic brain injuries. Most people understand that trauma exposure is a popular occupational hazard for military members. Psychiatric screenings, before and during their enlistment, and treatments after being exposed to warfare, death, destruction, and torture have been extremely beneficial for military personnel and their dependents.
A mental health professional is a health care practitioner or social and human services provider who offers services for the purpose of improving an individual's mental health or to treat mental disorders. This broad category was developed as a name for community personnel who worked in the new community mental health agencies begun in the 1970s to assist individuals moving from state hospitals, to prevent admissions, and to provide support in homes, jobs, education, and community. These individuals were the forefront brigade to develop the community programs, which today may be referred to by names such as supported housing, psychiatric rehabilitation, supported or transitional employment, sheltered workshops, supported education, daily living skills, affirmative industries, dual diagnosis treatment, individual and family psychoeducation, adult day care, foster care, family services and mental health counseling.

The Madigan Army Medical Center, located on Joint Base Lewis-McChord just outside Lakewood, Washington, is a key component of the Madigan Healthcare System and one of the largest military hospitals on the West Coast of the United States.

As defined by the United States Department of Veterans Affairs, military sexual trauma (MST) are experiences of sexual assault, or repeated threatening sexual harassment that occurred while a person was in the United States Armed Forces.

Lexington Veterans Affairs Medical Center, located in Lexington, Kentucky, is 199 bed medical facility owned by the United States Department of Veterans Affairs. The Lexington Veterans Affairs Medical Center is a fully accredited, two-division, tertiary care medical center with an operating bed complement of 199 hospital beds. Acute medical, neurological, surgical and psychiatric inpatient services are provided at the Cooper Division, located adjacent to the University of Kentucky Medical Center. Other available services include: emergency care, medical-surgical units, acute psychiatry, ICU, progressive care unit, ambulatory surgery, OR/PACU, hemodialysis, medicine specialty clinics, surgery specialty clinics, and outpatient primary and specialty care.
Psychiatry is the medical specialty devoted to the diagnosis, prevention, and treatment of deleterious mental conditions. These include various matters related to mood, behaviour, cognition, and perceptions.
The Norwegian Centre for Violence and Traumatic Stress Studies is a research centre in Oslo, Norway, and Norway's national research institution in violence and sexual abuse; disaster management, terrorism, armed conflicts and traumatic stress; and forced migration and refugee health research. It is interdisciplinary and employs experts mainly in psychology, psychiatry, and the social sciences. In addition to carrying out research and related activities, the institute advises the Government of Norway in its areas of expertise and has some official emergency management functions at the national level. NKVTS has 101 employees.
Addiction psychiatry is a medical subspecialty within psychiatry that focuses on the evaluation, diagnosis, and treatment of people who have one or more disorders related to addiction. This may include disorders involving legal and illegal drugs, gambling, sex, food, and other impulse control disorders. Addiction psychiatrists are substance use disorder experts. Growing amounts of scientific knowledge, such as the health effects and treatments for substance use disorders, have led to advancements in the field of addiction psychiatry. These advancements in understanding the neurobiology of rewarding behavior, along with federal funding, has allowed for ample opportunity for research in the discipline of addiction psychiatry. Addiction psychiatry is an expanding field, and currently there is a high demand for substance use disorder experts in both the private and public sector.

The United States has compensated military veterans for service-related injuries since the Revolutionary War, with the current indemnity model established near the end of World War I. The Department of Veterans Affairs (VA) began to provide disability benefits for post-traumatic stress disorder (PTSD) in the 1980s after the diagnosis became part of official psychiatric nosology.
The following outline is provided as an overview of and topical guide to psychiatry:
The Center for Deployment Psychology (CDP) is an organization offering training for behavioral health professionals who provide mental health services unique to the experience of deployment in the United States Armed Forces for active-duty military service members, veterans and their families. CDP is headquartered at the Uniformed Services University of the Health Sciences (USUHS) in Bethesda, Maryland, and is funded by the United States Department of Defense.
Bartley Christopher Frueh is a clinical psychologist and American author.
Operational stress injury or OSI is a non-clinical, non-medical term referring to a persistent psychological difficulty caused by traumatic experiences or prolonged high stress or fatigue during service as a military member or first responder. The term does not replace any individual diagnoses or disorders, but rather describes a category of mental health concerns linked to the particular challenges that these military members or first responders encounter in their service. There is not yet a single fixed definition. The term was first conceptualized within the Canadian Armed Forces to help foster understanding of the broader mental health challenges faced by military members who have been impacted by traumatic experiences and who face difficulty as a result. OSI encompasses a number of the diagnoses found in the Diagnostic and Statistical Manual of Mental Disorders (DSM) classification system, with the common thread being a linkage to the operational experiences of the afflicted. The term has gained traction outside of the military community as an appropriate way to describe similar challenges suffered by those whose work regularly exposes them to trauma, particularly front line emergency first responders such as but not limited to police, firefighters, paramedics, correctional officers, and emergency dispatchers. The term, at present mostly used within Canada, is increasingly significant in the development of legislation, policy, treatments and benefits in the military and first responder communities.

Internet-based treatments for trauma survivors is a growing class of online treatments that allow for an individual who has experienced trauma to seek and receive treatment without needing to attend psychotherapy in person. The progressive movement to online resources and the need for more accessible mental health services has given rise to the creation of online-based interventions aimed to help those who have experienced traumatic events. Cognitive behavioral therapy (CBT) has shown to be particularly effective in the treatment of trauma-related disorders and adapting CBT to an online format has been shown to be as effective as in-person CBT in the treatment of trauma. Due to its positive outcomes, CBT-based internet treatment options for trauma survivors has been an expanding field in both research and clinical settings.
References
Works cited
- 1 2 Temple, M. & Greenberg, N. (2002). Military psychiatry Archived 2007-02-10 at the Wayback Machine . British Medical Journal Career Focus, 324, S161a.
- ↑ Walter Reed Army Institute of Research-Psychiatry and Neuroscience. (2006, August 16). Department of Military Psychiatry. Retrieved November 03, 2007, from "Department of Military Psychiatry". Archived from the original on 2007-07-30. Retrieved 2007-11-03.
- ↑ Menninger, William C. (1967). A psychiatrist for a troubled world: selected papers . Viking Press. p. 495 . Retrieved June 12, 2012.
- ↑ Ulrik Malt (3 November 2017). "Arne Sund". Store norske leksikon . Retrieved 10 February 2019.
- ↑ "Eligibility | TRICARE". www.tricare.mil. Retrieved 2018-04-25.
- ↑ "Getting Mental Health Care | TRICARE". www.tricare.mil. Retrieved 2018-04-25.
- ↑ "Mental Health". Vets.gov. 2017-06-28. Retrieved 2018-04-25.
- 1 2 3 Ellard, J. (2000) "Principles of military psychiatry". Journal of the Australian Defence Health Services, 1, 81–84.
Other sources
- Jones, Franklin D., et al. (eds), Military Psychiatry: Preparing in Peace for War (1994; Series: Textbook of Military Medicine) – Explores various mental health issues that may occur in the military during peacetime: 331 pp.
- Jones, Franklin D., et al. (eds), War Psychiatry (1995; Series: Textbook of Military Medicine) - Discusses the evolution of the concept of combat stress reaction, the delivery of mental health care on the various battlefields soldiers are likely to experience, and the psychological consequences of having endured the intensity and lethality of modern combat: 515 pp.
- Shephard, Ben, A War of Nerves: Soldiers and Psychiatrists in the Twentieth Century (2000)