Related Research Articles
Obstetrics is the field of study concentrated on pregnancy, childbirth and the postpartum period. As a medical specialty, obstetrics is combined with gynecology under the discipline known as obstetrics and gynecology (OB/GYN), which is a surgical field.

Intrauterine growth restriction (IUGR), or fetal growth restriction, is the poor growth of a fetus while in the womb during pregnancy. IUGR is defined by clinical features of malnutrition and evidence of reduced growth regardless of an infant's birth weight percentile. The causes of IUGR are broad and may involve maternal, fetal, or placental complications.

Eclampsia is the onset of seizures (convulsions) in a woman with pre-eclampsia. Pre-eclampsia is a hypertensive disorder of pregnancy that presents with three main features: new onset of high blood pressure, large amounts of protein in the urine or other organ dysfunction, and edema. If left untreated, pre-eclampsia can result in long-term consequences for the mother, namely increased risk of cardiovascular diseases and associated complications. In more severe cases, it may be fatal for both the mother and the fetus.

Pre-eclampsia is a multi-system disorder specific to pregnancy, characterized by the onset of high blood pressure and often a significant amount of protein in the urine. When it arises, the condition begins after 20 weeks of pregnancy. In severe cases of the disease there may be red blood cell breakdown, a low blood platelet count, impaired liver function, kidney dysfunction, swelling, shortness of breath due to fluid in the lungs, or visual disturbances. Pre-eclampsia increases the risk of undesirable as well as lethal outcomes for both the mother and the fetus including preterm labor. If left untreated, it may result in seizures at which point it is known as eclampsia.
Fetal distress, also known as non-reassuring fetal status, is a condition during pregnancy or labor in which the fetus shows signs of inadequate oxygenation. Due to its imprecision, the term "fetal distress" has fallen out of use in American obstetrics. The term "non-reassuring fetal status" has largely replaced it. It is characterized by changes in fetal movement, growth, heart rate, and presence of meconium stained fluid.

Prenatal testing is a tool that can be used to detect some birth defects at various stages prior to birth. Prenatal testing consists of prenatal screening and prenatal diagnosis, which are aspects of prenatal care that focus on detecting problems with the pregnancy as early as possible. These may be anatomic and physiologic problems with the health of the zygote, embryo, or fetus, either before gestation even starts or as early in gestation as practicable. Screening can detect problems such as neural tube defects, chromosome abnormalities, and gene mutations that would lead to genetic disorders and birth defects, such as spina bifida, cleft palate, Down syndrome, trisomy 18, Tay–Sachs disease, sickle cell anemia, thalassemia, cystic fibrosis, muscular dystrophy, and fragile X syndrome. Some tests are designed to discover problems which primarily affect the health of the mother, such as PAPP-A to detect pre-eclampsia or glucose tolerance tests to diagnose gestational diabetes. Screening can also detect anatomical defects such as hydrocephalus, anencephaly, heart defects, and amniotic band syndrome.

Gestational hypertension or pregnancy-induced hypertension (PIH) is the development of new hypertension in a pregnant woman after 20 weeks' gestation without the presence of protein in the urine or other signs of pre-eclampsia. Gestational hypertension is defined as having a blood pressure greater than 140/90 on two occasions at least 6 hours apart.
Oligohydramnios is a medical condition in pregnancy characterized by a deficiency of amniotic fluid, the fluid that surrounds the fetus in the abdomen, in the amniotic sac. The limiting case is anhydramnios, where there is a complete absence of amniotic fluid. It is typically diagnosed by ultrasound when the amniotic fluid index (AFI) measures less than 5 cm or when the single deepest pocket (SDP) of amniotic fluid measures less than 2 cm. Amniotic fluid is necessary to allow for normal fetal movement, lung development, and cushioning from uterine compression. Low amniotic fluid can be attributed to a maternal, fetal, placental or idiopathic cause and can result in poor fetal outcomes including death. The prognosis of the fetus is dependent on the etiology, gestational age at diagnosis, and the severity of the oligohydramnios.

Hydrops fetalis or hydrops foetalis is a condition in the fetus characterized by an accumulation of fluid, or edema, in at least two fetal compartments. By comparison, hydrops allantois or hydrops amnion is an accumulation of excessive fluid in the allantoic or amniotic space, respectively.

Complications of pregnancy are health problems that are related to, or arise during pregnancy. Complications that occur primarily during childbirth are termed obstetric labor complications, and problems that occur primarily after childbirth are termed puerperal disorders. While some complications improve or are fully resolved after pregnancy, some may lead to lasting effects, morbidity, or in the most severe cases, maternal or fetal mortality.

Intrauterine hypoxia occurs when the fetus is deprived of an adequate supply of oxygen. It may be due to a variety of reasons such as prolapse or occlusion of the umbilical cord, placental infarction, maternal diabetes and maternal smoking. Intrauterine growth restriction may cause or be the result of hypoxia. Intrauterine hypoxia can cause cellular damage that occurs within the central nervous system. This results in an increased mortality rate, including an increased risk of sudden infant death syndrome (SIDS). Oxygen deprivation in the fetus and neonate have been implicated as either a primary or as a contributing risk factor in numerous neurological and neuropsychiatric disorders such as epilepsy, attention deficit hyperactivity disorder, eating disorders and cerebral palsy.

Placenta accreta occurs when all or part of the placenta attaches abnormally to the myometrium. Three grades of abnormal placental attachment are defined according to the depth of attachment and invasion into the muscular layers of the uterus:
- Accreta – chorionic villi attached to the myometrium, rather than being restricted within the decidua basalis.
- Increta – chorionic villi invaded into the myometrium.
- Percreta – chorionic villi invaded through the perimetrium.

Uterine atony is the failure of the uterus to contract adequately following delivery. Contraction of the uterine muscles during labor compresses the blood vessels and slows flow, which helps prevent hemorrhage and facilitates coagulation. Therefore, a lack of uterine muscle contraction can lead to an acute hemorrhage, as the vasculature is not being sufficiently compressed. Uterine atony is the most common cause of postpartum hemorrhage, which is an emergency and potential cause of fatality. Across the globe, postpartum hemorrhage is among the top five causes of maternal death. Recognition of the warning signs of uterine atony in the setting of extensive postpartum bleeding should initiate interventions aimed at regaining stable uterine contraction.

Kyprianos "Kypros" Nicolaides is a Greek Cypriot physician of British citizenship, Professor of Fetal Medicine at King's College Hospital, London. He is one of the pioneers of fetal medicine and his discoveries have revolutionised the field. He was elected to the US National Academy of Medicine in 2020 for 'improving the care of pregnant women worldwide with pioneering rigorous and creative approaches, and making seminal contributions to prenatal diagnosis and every major obstetrical disorder'. This is considered to be one of the highest honours in the fields of health and medicine and recognises individuals who have demonstrated outstanding professional achievement and commitment to service.
Hemoglobin Barts, abbreviated Hb Barts, is an abnormal type of hemoglobin that consists of four gamma globins. It is moderately insoluble, and therefore accumulates in the red blood cells. Hb Barts has an extremely high affinity for oxygen, so it cannot release oxygen to the tissue. Therefore, this makes it an inefficient oxygen carrier. As an embryo develops, it begins to produce alpha-globins at weeks 5–6 of development. When both of the HBA1 and HBA2 genes which code for alpha globins becomes dysfunctional, the affected fetuses will have difficulty in synthesizing a functional hemoglobin. As a result, gamma chains will accumulate and form four gamma globins. These gamma globins bind to form hemoglobin Barts. It is produced in the disease alpha-thalassemia and in the most severe of cases, it is the only form of hemoglobin in circulation. In this situation, a fetus will develop hydrops fetalis and normally die before or shortly after birth, unless intrauterine blood transfusion is performed.

Velamentous cord insertion is a complication of pregnancy where the umbilical cord is inserted in the fetal membranes. It is a major cause of antepartum hemorrhage that leads to loss of fetal blood and associated with high perinatal mortality. In normal pregnancies, the umbilical cord inserts into the middle of the placental mass and is completely encased by the amniotic sac. The vessels are hence normally protected by Wharton's jelly, which prevents rupture during pregnancy and labor. In velamentous cord insertion, the vessels of the umbilical cord are improperly inserted in the chorioamniotic membrane, and hence the vessels traverse between the amnion and the chorion towards the placenta. Without Wharton's jelly protecting the vessels, the exposed vessels are susceptible to compression and rupture.

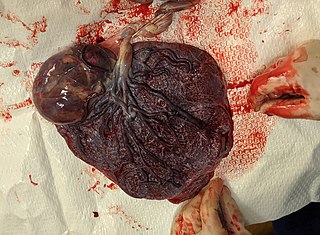
A placental disease is any disease, disorder, or pathology of the placenta.
Cell-free fetal DNA (cffDNA) is fetal DNA that circulates freely in the maternal blood. Maternal blood is sampled by venipuncture. Analysis of cffDNA is a method of non-invasive prenatal diagnosis frequently ordered for pregnant women of advanced maternal age. Two hours after delivery, cffDNA is no longer detectable in maternal blood.
Hypertensive disease of pregnancy, also known as maternal hypertensive disorder, is a group of high blood pressure disorders that include preeclampsia, preeclampsia superimposed on chronic hypertension, gestational hypertension, and chronic hypertension.
Chorioangioma, or chorangioma, is a benign tumor of placenta. It is a hamartoma-like growth in the placenta consisting of blood vessels, and is seen in approximately 0.5 to 1% pregnancies. It is mostly diagnosed ultrasonically in the second trimester of pregnancy. Large chorioangiomas are known to cause complications in pregnancy, while the smaller ones are asymptomatic.
References
- 1 2 Paternoster DM, Manganelli F, Minucci D, Nanhornguè KN, Memmo A, Bertoldini M, Nicolini U (2006). "Ballantyne Syndrome: a Case Report". Fetal Diagnosis and Therapy. 21 (1): 92–5. doi:10.1159/000089056. PMID 16354984. S2CID 36608058.
- ↑ "Ballantyne's syndrome".
- ↑ Vidaeff AC, Pschirrer ER, Mastrobattista JM, Gilstrap LC, Ramin SM (2002). "Mirror syndrome. A case report". The Journal of Reproductive Medicine. 47 (9): 770–4. PMID 12380459.
- ↑ Chang YL, Chao AS, Hsu JJ, Chang SD, Soong YK (2007). "Selective fetocide reversed mirror syndrome in a dichorionic triplet pregnancy with severe twin-twin transfusion syndrome: a case report". Fetal Diagn. Ther. 22 (6): 428–30. doi:10.1159/000106348. PMID 17652930. S2CID 21536375.
- ↑ Balakumar K (2003). "Antenatal diagnosis of vein of Galen aneurysm: case report". Indian Journal of Radiology and Imaging. 13 (1): 91–2. Archived from the original on 2018-05-27. Retrieved 2011-03-31.
- ↑ Carbillon L, Oury JF, Guerin JM, Azancot A, Blot P (1997). "Clinical biological features of Ballantyne syndrome and the role of placental hydrops". Obstetrical & Gynecological Survey. 52 (5): 310–4. doi:10.1097/00006254-199705000-00023. PMID 9140132.
- ↑ Machado LE, Osborne NG, Bonilla-Musoles F (2002). "Two-dimensional and three-dimensional ultrasound of fetal (baby) anasarca: the glass baby". Journal of Perinatal Medicine. 30 (1): 105–10. doi:10.1515/JPM.2002.013. PMID 11933650. S2CID 26606491.
- 1 2 Van Selm M, Kanhai HH, Gravenhorst JB (1991). "Maternal hydrops syndrome: a review". Obstetrical & Gynecological Survey. 46 (12): 785–8. doi:10.1097/00006254-199112000-00001. PMID 1780115.
- ↑ "Archived copy" (PDF). sogc.org. Archived from the original (PDF) on 27 August 2014. Retrieved 22 May 2022.
{{cite web}}: CS1 maint: archived copy as title (link) - ↑ Pirhonen JP, Hartgil TW (2004). "Spontaneous reversal of mirror syndrome in a twin pregnancy after a single fetal death". European Journal of Obstetrics & Gynecology and Reproductive Biology. 116 (1): 106–7. doi:10.1016/j.ejogrb.2003.12.011. PMID 15294378.
- ↑ Gherman RB, Incerpi MH, Wing DA, Goodwin TM (1998). "Ballantyne syndrome: is placental ischemia the etiology?". Journal of Maternal-Fetal Medicine. 7 (5): 227–9. doi:10.1002/(SICI)1520-6661(199809/10)7:5<227::AID-MFM3>3.0.CO;2-I. PMID 9775990.
- ↑ Heyborne KD, Chism DM (2000). "Reversal of Ballantyne syndrome by selective second-trimester fetal termination. A case report". Journal of Reproductive Medicine. 45 (4): 360–2. PMID 10804498.
- ↑ Midgley DY, Harding K (2000). "The mirror syndrome". European Journal of Obstetrics & Gynecology and Reproductive Biology. 88 (2): 201–2. doi:10.1016/S0301-2115(99)00147-5. PMID 10690681.