Paralysis is a loss of motor function in one or more muscles. Paralysis can also be accompanied by a loss of feeling in the affected area if there is sensory damage. In the United States, roughly 1 in 50 people have been diagnosed with some form of permanent or transient paralysis. The word "paralysis" derives from the Greek παράλυσις, meaning "disabling of the nerves" from παρά (para) meaning "beside, by" and λύσις (lysis) meaning "making loose". A paralysis accompanied by involuntary tremors is usually called "palsy".

Syringomyelia is a generic term referring to a disorder in which a cyst or cavity forms within the spinal cord. Often, syringomyelia is used as a generic term before an etiology is determined. This cyst, called a syrinx, can expand and elongate over time, destroying the spinal cord. The damage may result in loss of feeling, paralysis, weakness, and stiffness in the back, shoulders, and extremities. Syringomyelia may also cause a loss of the ability to feel extremes of hot or cold, especially in the hands. It may also lead to a cape-like bilateral loss of pain and temperature sensation along the upper chest and arms. The combination of symptoms varies from one patient to another depending on the location of the syrinx within the spinal cord, as well as its extent.

Transverse myelitis (TM) is a rare neurological condition wherein the spinal cord is inflamed. The adjective transverse implies that the spinal inflammation (myelitis) extends horizontally throughout the cross section of the spinal cord; the terms partial transverse myelitis and partial myelitis are sometimes used to specify inflammation that affects only part of the width of the spinal cord. TM is characterized by weakness and numbness of the limbs, deficits in sensation and motor skills, dysfunctional urethral and anal sphincter activities, and dysfunction of the autonomic nervous system that can lead to episodes of low blood pressure and Dizziness. Signs and symptoms vary according to the affected level of the spinal cord. The underlying cause of TM is unknown. The spinal cord inflammation seen in TM has been associated with various infections, immune system disorders, or damage to nerve fibers, by loss of myelin. As opposed to leukomyelitis which affects only the white matter, it affects the entire cross-section of the spinal cord. Decreased electrical conductivity in the nervous system can result.

Tetraplegia, also known as quadriplegia, is defined as the dysfunction or loss of motor and/or sensory function in the cervical area of the spinal cord. A loss of motor function can present as either weakness or paralysis leading to partial or total loss of function in the arms, legs, trunk, and pelvis; paraplegia is similar but affects the thoracic, lumbar, and sacral segments of the spinal cord and arm function is retained. The paralysis may be flaccid or spastic. A loss of sensory function can present as an impairment or complete inability to sense light touch, pressure, heat, pinprick/pain, and proprioception. In these types of spinal cord injury, it is common to have a loss of both sensation and motor control.
Myelitis is inflammation of the spinal cord which can disrupt the normal responses from the brain to the rest of the body, and from the rest of the body to the brain. Inflammation in the spinal cord can cause the myelin and axon to be damaged resulting in symptoms such as paralysis and sensory loss. Myelitis is classified to several categories depending on the area or the cause of the lesion; however, any inflammatory attack on the spinal cord is often referred to as transverse myelitis.
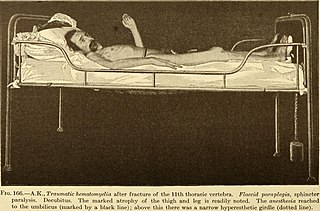
Paraplegia, or paraparesis, is an impairment in motor or sensory function of the lower extremities. The word comes from Ionic Greek (παραπληγίη) "half-stricken". It is usually caused by spinal cord injury or a congenital condition that affects the neural (brain) elements of the spinal canal. The area of the spinal canal that is affected in paraplegia is either the thoracic, lumbar, or sacral regions. If four limbs are affected by paralysis, tetraplegia or quadriplegia is the correct term. If only one limb is affected, the correct term is monoplegia. Spastic paraplegia is a form of paraplegia defined by spasticity of the affected muscles, rather than flaccid paralysis.

Spondylosis is the degeneration of the vertebral column from any cause. In the more narrow sense it refers to spinal osteoarthritis, the age-related degeneration of the spinal column, which is the most common cause of spondylosis. The degenerative process in osteoarthritis chiefly affects the vertebral bodies, the neural foramina and the facet joints. If severe, it may cause pressure on the spinal cord or nerve roots with subsequent sensory or motor disturbances, such as pain, paresthesia, imbalance, and muscle weakness in the limbs.

A spinal cord injury (SCI) is damage to the spinal cord that causes temporary or permanent changes in its function. Symptoms may include loss of muscle function, sensation, or autonomic function in the parts of the body served by the spinal cord below the level of the injury. Injury can occur at any level of the spinal cord and can be complete, with a total loss of sensation and muscle function at lower sacral segments, or incomplete, meaning some nervous signals are able to travel past the injured area of the cord up to the Sacral S4-5 spinal cord segments. Depending on the location and severity of damage, the symptoms vary, from numbness to paralysis, including bowel or bladder incontinence. Long term outcomes also range widely, from full recovery to permanent tetraplegia or paraplegia. Complications can include muscle atrophy, loss of voluntary motor control, spasticity, pressure sores, infections, and breathing problems.
Myelopathy describes any neurologic deficit related to the spinal cord. The most common form of myelopathy in humans, cervical spondylotic myelopathy (CSM), also called degenerative cervical myelopathy, results from narrowing of the spinal canal ultimately causing compression of the spinal cord. When due to trauma, myelopathy is known as (acute) spinal cord injury. When inflammatory, it is known as myelitis. Disease that is vascular in nature is known as vascular myelopathy.
Monoplegia is paralysis of a single limb, usually an arm. Common symptoms associated with monoplegic patients are weakness, numbness, and pain in the affected limb. Monoplegia is a type of paralysis that falls under hemiplegia. While hemiplegia is paralysis of half of the body, monoplegia is localized to a single limb or to a specific region of the body. Monoplegia of the upper limb is sometimes referred to as brachial monoplegia, and that of the lower limb is called crural monoplegia. Monoplegia in the lower extremities is not as common of an occurrence as in the upper extremities. Monoparesis is a similar, but less severe, condition because one limb is very weak, not paralyzed. For more information, see paresis.

A spinal disc herniation is an injury to the intervertebral disc between two spinal vertebrae, usually caused by excessive strain or trauma to the spine. It may result in back pain, pain or sensation in different parts of the body, and physical disability. The most conclusive diagnostic tool for disc herniation is MRI, and treatment may range from painkillers to surgery. Protection from disc herniation is best provided by core strength and an awareness of body mechanics including good posture.

Anterior spinal artery syndrome is syndrome caused by ischemia of the area supplied by the anterior spinal artery, resulting in loss of function of the anterior two-thirds of the spinal cord. The region affected includes the descending corticospinal tract, ascending spinothalamic tract, and autonomic fibers. It is characterized by a corresponding loss of motor function, loss of pain and temperature sensation, and hypotension.

Central cord syndrome (CCS) is the most common form of cervical spinal cord injury. It is characterized by loss of power and sensation in arms and hands. It usually results from trauma which causes damage to the neck, leading to major injury to the central corticospinal tract of the spinal cord. CCS most frequently occurs among older persons with cervical spondylosis, however, it also may occur in younger individuals.

Brown-Séquard syndrome is caused by damage to one half of the spinal cord, i.e. hemisection of the spinal cord resulting in paralysis and loss of proprioception on the same side as the injury or lesion, and loss of pain and temperature sensation on the opposite side as the lesion. It is named after physiologist Charles-Édouard Brown-Séquard, who first described the condition in 1850.
Vascular myelopathy refers to an abnormality of the spinal cord in regard to its blood supply. The blood supply is complicated and supplied by two major vessel groups: the posterior spinal arteries and the anterior spinal arteries—of which the Artery of Adamkiewicz is the largest. Both the posterior and anterior spinal arteries run the entire length of the spinal cord and receive anastomotic (conjoined) vessels in many places. The anterior spinal artery has a less efficient supply of blood and is therefore more susceptible to vascular disease. Whilst atherosclerosis of spinal arteries is rare, necrosis in the anterior artery can be caused by disease in vessels originating from the segmental arteries such as atheroma or aortic dissection.

Metrizamide is a non-ionic iodine-based radiocontrast agent. It is also a density gradient medium for the centrifugation of biological particles.

The spinal cord is a long, thin, tubular structure made up of nervous tissue that extends from the medulla oblongata in the brainstem to the lumbar region of the vertebral column (backbone) of vertebrate animals. The center of the spinal cord is hollow and contains a structure called central canal, which contains cerebrospinal fluid. The spinal cord is also covered by meninges and enclosed by the neural arches. Together, the brain and spinal cord make up the central nervous system.

A lumbar anterior root stimulator is a type of neuroprosthesis used in patients with a spinal cord injury or to treat some forms of chronic spinal pain. More specifically, the root stimulator can be used in patients who have lost proper bowel function due to damaged neurons related to gastrointestinal control and potentially allow paraplegics to exercise otherwise paralyzed leg muscles.
Spinal cord injury research seeks new ways to cure or treat spinal cord injury in order to lessen the debilitating effects of the injury in the short or long term. There is no cure for SCI, and current treatments are mostly focused on spinal cord injury rehabilitation and management of the secondary effects of the condition. Two major areas of research include neuroprotection, ways to prevent damage to cells caused by biological processes that take place in the body after the injury, and neuroregeneration, regrowing or replacing damaged neural circuits.
Spinal cord stroke is a rare type of stroke with compromised blood flow to any region of spinal cord owing to occlusion or bleeding, leading to irreversible neuronal death. It can be classified into two types, ischaemia and haemorrhage, in which the former accounts for 86% of all cases, a pattern similar to cerebral stroke. The disease is either arisen spontaneously from aortic illnesses or postoperatively. It deprives patients of motor function or sensory function, and sometimes both. Infarction usually occurs in regions perfused by anterior spinal artery, which spans the anterior two-thirds of spinal cord. Preventions of the disease include decreasing the risk factors and maintaining enough spinal cord perfusion pressure during and after the operation. The process of diagnosing the ischemic and hemorrhagic spinal cord stroke includes applying different MRI protocols and CT scan. Treatments for spinal cord stroke are mainly determined by the symptoms and the causes of the disease. For example, antiplatelet and corticosteroids might be used to reduce the risk of blood clots in ischaemic spinal stroke patients, while rapid surgical decompression is applied to minimize neurological injuries in haemorrhagic spinal stroke patients instead. Patients may spend years for rehabilitation after the spinal cord stroke.