The peripheral nervous system (PNS) is one of two components that make up the nervous system of bilateral animals, with the other part being the central nervous system (CNS). The PNS consists of nerves and ganglia, which lie outside the brain and the spinal cord. The main function of the PNS is to connect the CNS to the limbs and organs, essentially serving as a relay between the brain and spinal cord and the rest of the body. Unlike the CNS, the PNS is not protected by the vertebral column and skull, or by the blood–brain barrier, which leaves it exposed to toxins.
Articles related to anatomy include:

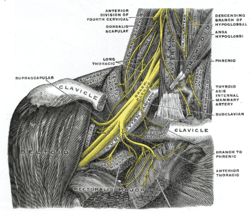
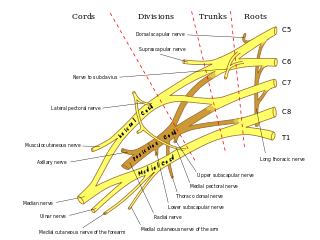
The brachial plexus is a network of nerves formed by the anterior rami of the lower four cervical nerves and first thoracic nerve. This plexus extends from the spinal cord, through the cervicoaxillary canal in the neck, over the first rib, and into the armpit, it supplies afferent and efferent nerve fibers to the chest, shoulder, arm, forearm, and hand.

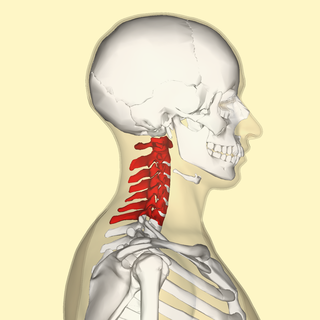
A spinal nerve is a mixed nerve, which carries motor, sensory, and autonomic signals between the spinal cord and the body. In the human body there are 31 pairs of spinal nerves, one on each side of the vertebral column. These are grouped into the corresponding cervical, thoracic, lumbar, sacral and coccygeal regions of the spine. There are eight pairs of cervical nerves, twelve pairs of thoracic nerves, five pairs of lumbar nerves, five pairs of sacral nerves, and one pair of coccygeal nerves. The spinal nerves are part of the peripheral nervous system.

In human anatomy, the subclavian arteries are paired major arteries of the upper thorax, below the clavicle. They receive blood from the aortic arch. The left subclavian artery supplies blood to the left arm and the right subclavian artery supplies blood to the right arm, with some branches supplying the head and thorax. On the left side of the body, the subclavian comes directly off the aortic arch, while on the right side it arises from the relatively short brachiocephalic artery when it bifurcates into the subclavian and the right common carotid artery.

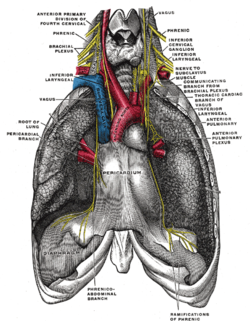
The cervical plexus is a nerve plexus of the anterior rami of the first four cervical spinal nerves C1-C4. The cervical plexus provides motor innervation to some muscles of the neck, and the diaphragm; it provides sensory innervation to parts of the head, neck, and chest.
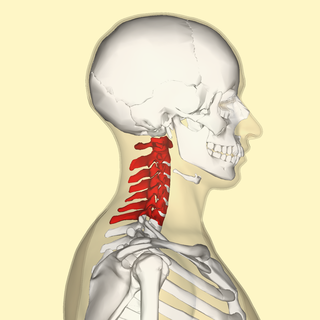
In tetrapods, cervical vertebrae are the vertebrae of the neck, immediately below the skull. Truncal vertebrae lie caudal of cervical vertebrae. In sauropsid species, the cervical vertebrae bear cervical ribs. In lizards and saurischian dinosaurs, the cervical ribs are large; in birds, they are small and completely fused to the vertebrae. The vertebral transverse processes of mammals are homologous to the cervical ribs of other amniotes. Most mammals have seven cervical vertebrae, with the only three known exceptions being the manatee with six, the two-toed sloth with five or six, and the three-toed sloth with nine.

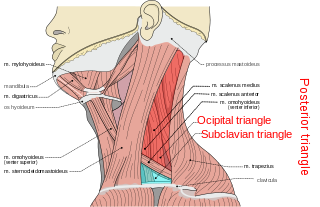
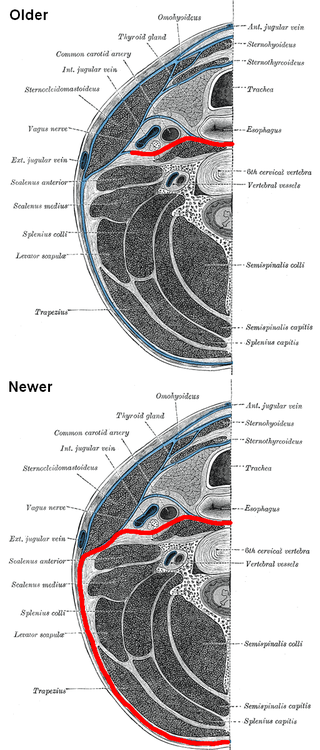
The scalene muscles are a group of three muscles on each side of the neck, identified as the anterior, the middle, and the posterior. They are innervated by the third to the eighth cervical spinal nerves (C3-C8).

The ansa cervicalis is a loop formed by muscular branches of the cervical plexus formed by branches of cervical spinal nerves C1-C3. The ansa cervicalis has two roots - a superior root and an inferior root - that unite distally, forming a loop. It is situated within the carotid sheath.

A nerve plexus is a plexus of intersecting nerves. A nerve plexus is composed of afferent and efferent fibers that arise from the merging of the anterior rami of spinal nerves and blood vessels. There are five spinal nerve plexuses, except in the thoracic region, as well as other forms of autonomic plexuses, many of which are a part of the enteric nervous system. The nerves that arise from the plexuses have both sensory and motor functions. These functions include muscle contraction, the maintenance of body coordination and control, and the reaction to sensations such as heat, cold, pain, and pressure. There are several plexuses in the body, including:

The thoracic aorta is a part of the aorta located in the thorax. It is a continuation of the aortic arch. It is located within the posterior mediastinal cavity, but frequently bulges into the left pleural cavity. The descending thoracic aorta begins at the lower border of the fourth thoracic vertebra and ends in front of the lower border of the twelfth thoracic vertebra, at the aortic hiatus in the diaphragm where it becomes the abdominal aorta.
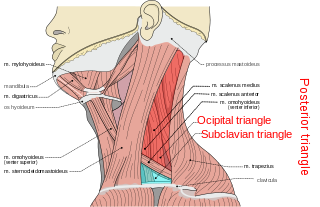
The posterior triangle is a region of the neck.

The pericardiacophrenic artery is a long slender branch of the internal thoracic artery.
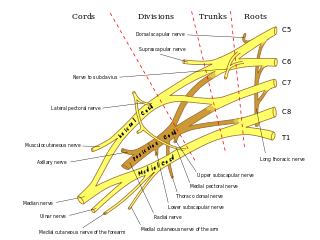
The subclavian nerve, also known as the nerve to the subclavius, is a small branch of the upper trunk of the brachial plexus. It contains axons from C5 and C6. It innervates the subclavius muscle.

The subclavian triangle, the smaller division of the posterior triangle, is bounded, above, by the inferior belly of the omohyoideus; below, by the clavicle; its base is formed by the posterior border of the sternocleidomastoideus.

This article describes the anatomy of the head and neck of the human body, including the brain, bones, muscles, blood vessels, nerves, glands, nose, mouth, teeth, tongue, and throat.

The ventral ramus is the anterior division of a spinal nerve. The ventral rami supply the antero-lateral parts of the trunk and the limbs. They are mainly larger than the dorsal rami.
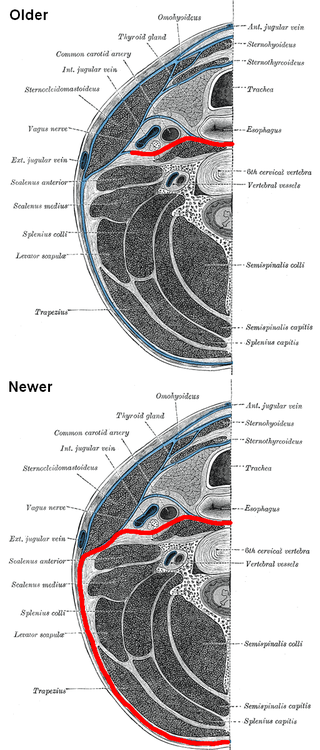
The prevertebral fascia is the layer of deep cervical fascia that surrounds the vertebral column. It is the deepest layer of deep cervical fascia.

The following outline is provided as an overview of and topical guide to human anatomy:

The pulmonary pleurae are the two flattened sacs ensheathing each lung, locally appearing as two opposing layers of serous membrane separating the lungs from the mediastinum and the inside surfaces of the surrounding chest walls.