Absorption
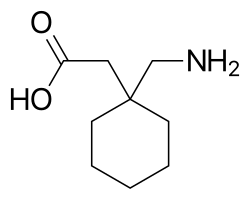
Gabapentin and pregabalin are absorbed from the intestines by an active transport process mediated via the large neutral amino acid transporter 1 (LAT1, SLC7A5), a transporter for amino acids such as L-leucine and L-phenylalanine. [1] [15] [22] Very few (less than 10 drugs) are known to be transported by this transporter. [23] Unlike gabapentin, which is transported solely by the LAT1, [22] [24] pregabalin seems to be transported not only by the LAT1 but also by other carriers. [1] The LAT1 is easily saturable, so the pharmacokinetics of gabapentin are dose-dependent, with diminished bioavailability and delayed peak levels at higher doses. [1] Conversely, this is not the case for pregabalin, which shows linear pharmacokinetics and no saturation of absorption. [1] Similarly, gabapentin enacarbil is transported not by the LAT1 but by the monocarboxylate transporter 1 (MCT1) and the sodium-dependent multivitamin transporter (SMVT), and no saturation of bioavailability has been observed with the drug up to a dose of 2,800 mg. [25] Similarly to gabapentin and pregabalin, baclofen, a close analogue of phenibut (baclofen specifically being 4-chlorophenibut), is transported by the LAT1, although it is a relatively weak substrate for the transporter. [23] [26]
The oral bioavailability of gabapentin is approximately 80% at 100 mg administered three times daily once every 8 hours, but decreases to 60% at 300 mg, 47% at 400 mg, 34% at 800 mg, 33% at 1,200 mg, and 27% at 1,600 mg, all with the same dosing schedule. [24] [25] Conversely, the oral bioavailability of pregabalin is greater than or equal to 90% across and beyond its entire clinical dose range (75 to 900 mg/day). [24] Food does not significantly influence the oral bioavailability of pregabalin. [24] Conversely, food increases the area-under-curve levels of gabapentin by about 10%. [24] Drugs that increase the transit time of gabapentin in the small intestine can increase its oral bioavailability; when gabapentin was co-administered with oral morphine (which slows intestinal peristalsis), [27] the oral bioavailability of a 600 mg dose of gabapentin increased by 50%. [24] The oral bioavailability of gabapentin enacarbil (as gabapentin) is greater than or equal to 68%, across all doses assessed (up to 2,800 mg), with a mean of approximately 75%. [25] [1] In contrast to the other gabapentinoids, the pharmacokinetics of phenibut have been little-studied, and its oral bioavailability is unknown. [28] However, it would appear to be at least 63% at a single dose of 250 mg, based on the fact that this fraction of phenibut was recovered from the urine unchanged in healthy volunteers administered this dose. [28]
Gabapentin at a low dose of 100 mg has a Tmax (time to peak levels) of approximately 1.7 hours, while the Tmax increases to 3 to 4 hours at higher doses. [1] The Tmax of pregabalin is generally less than or equal to 1 hour at doses of 300 mg or less. [1] However, food has been found to substantially delay the absorption of pregabalin and to significantly reduce peak levels without affecting the bioavailability of the drug; Tmax values for pregabalin of 0.6 hours in a fasted state and 3.2 hours in a fed state (5-fold difference), and the Cmax is reduced by 25–31% in a fed versus fasted state. [24] In contrast to pregabalin, food does not significantly affect the Tmax of gabapentin and increases the Cmax of gabapentin by approximately 10%. [24] The Tmax of the instant-release (IR) formulation of gabapentin enacarbil (as active gabapentin) is about 2.1 to 2.6 hours across all doses (350–2,800 mg) with single administration and 1.6 to 1.9 hours across all doses (350–2,100 mg) with repeated administration. [29] Conversely, the Tmax of the extended-release (XR) formulation of gabapentin enacarbil is about 5.1 hours at a single dose of 1,200 mg in a fasted state and 8.4 hours at a single dose of 1,200 mg in a fed state. [29] The Tmax of phenibut has not been reported, [28] but the onset of action and peak effects have been described as occurring at 2 to 4 hours and 5 to 6 hours, respectively, after oral ingestion in recreational users taking high doses (1–3 g). [30]
Distribution
Gabapentin, pregabalin, and phenibut all cross the blood–brain barrier and enter the central nervous system. [15] [28] However, due to their low lipophilicity, [24] the gabapentinoids require active transport across the blood–brain barrier. [22] [15] [31] [32] The LAT1 is highly expressed at the blood–brain barrier [33] and transports the gabapentinoids that bind to it across into the brain. [22] [15] [31] [32] As with intestinal absorption of gabapentin mediated by LAT1, transport of gabapentin across the blood–brain barrier by LAT1 is saturable. [22] Gabapentin does not bind to other drug transporters such as P-glycoprotein (ABCB1) or OCTN2 (SLC22A5). [22]
Gabapentin and pregabalin are not significantly bound to plasma proteins (<1%). [24] The phenibut analogue baclofen shows low plasma protein binding of 30%. [34]
Elimination
Gabapentin, pregabalin, and phenibut are all eliminated renally in the urine. [24] [28] They all have relatively short elimination half-lives, with reported values of 5.0 to 7.0 hours, 6.3 hours, and 5.3 hours, respectively. [24] [28] Similarly, the terminal half-life of gabapentin enacarbil IR (as active gabapentin) is short at approximately 4.5 to 6.5 hours. [29] Because of its short elimination half-life, gabapentin must be administered 3 to 4 times per day to maintain therapeutic levels. [25] Similarly, pregabalin has been given 2 to 3 times per day in clinical studies. [24] Phenibut, also, is taken 3 times per day. [35] [36] Conversely, gabapentin enacarbil is taken twice a day and gabapentin XR (brand name Gralise) is taken once a day. [37]