 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Stresam |
| Other names | Étifoxine; Etifoxin; Etafenoxine; Etafenoxin; EFX; Hoe 36801; Hoe-36,801 |
| AHFS/Drugs.com | International Drug Names |
| Pregnancy category |
|
| Routes of administration | Oral administration [2] |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 90% [3] |
| Protein binding | 88–95% [4] |
| Metabolism | Liver [5] |
| Metabolites | Several (including diethyletifoxine) [5] |
| Elimination half-life | Etifoxine: 6 hours [5] Diethyletifoxine: 20 hours [5] |
| Excretion | Mainly urine, also bile [5] [2] |
| Identifiers | |
| |
| CAS Number |
|
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.158.584 |
| Chemical and physical data | |
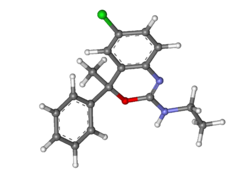
| Formula | C17H17ClN2O |
| Molar mass | 300.79 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Etifoxine, sold under the trade name Stresam among others, is a nonbenzodiazepine anxiolytic agent, primarily indicated for short-term management of adjustment disorder, specifically instances of situational depression accompanied by anxiety, such as stress-induced anxiety. [2] [6] Administration is by mouth. [7] Side effects associated with etifoxine use include slight drowsiness, headache, skin eruptions, and allergic reactions. [2] [8] [9] In rare cases, etifoxine has been linked to severe skin and liver toxicity, as well as menstrual bleeding between periods. [8] [1] Unlike benzodiazepines, etifoxine does not cause sedation or lack of coordination. [10] [3] Etifoxine acts as a ligand for translocator proteins. [10]
Contents
- Medical uses
- Available forms
- Contraindications
- Side effects
- Pharmacology
- Pharmacodynamics
- Pharmacokinetics
- Chemistry
- History
- Society and culture
- Names
- Availability
- See also
- References
- Further reading
- External links
Etifoxine was developed in the 1960s and was introduced for medical use in France in 1979. [11] Its marketed in 53 countries worldwide, although it remains unavailable in the United States. [7] [11] [12] Throughout the 2010s and early 2020s, the safety profile of etifoxine was scrutinized within France and the European Union, prompted by reports of toxicity. [13] [8] [7] The investigation revealed that instances of toxicity were infrequent, and etifoxine was allowed to remain on the market. [13] [8] [7]
