In humans, the kidneys are two reddish-brown bean-shaped blood-filtering organs that are a multilobar, multipapillary form of mammalian kidneys, usually without signs of external lobulation. They are located on the left and right in the retroperitoneal space, and in adult humans are about 12 centimetres in length. They receive blood from the paired renal arteries; blood exits into the paired renal veins. Each kidney is attached to a ureter, a tube that carries excreted urine to the bladder.

Creatinine is a breakdown product of creatine phosphate from muscle and protein metabolism. It is released at a constant rate by the body.
The excretory system is a passive biological system that removes excess, unnecessary materials from the body fluids of an organism, so as to help maintain internal chemical homeostasis and prevent damage to the body. The dual function of excretory systems is the elimination of the waste products of metabolism and to drain the body of used up and broken down components in a liquid and gaseous state. In humans and other amniotes, most of these substances leave the body as urine and to some degree exhalation, mammals also expel them through sweating.
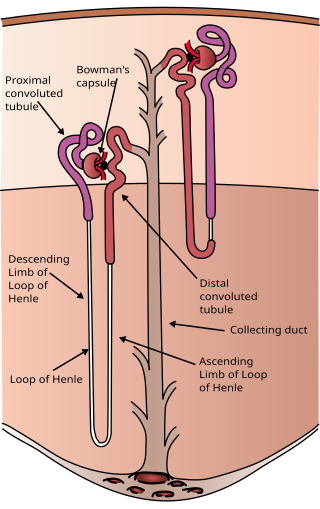
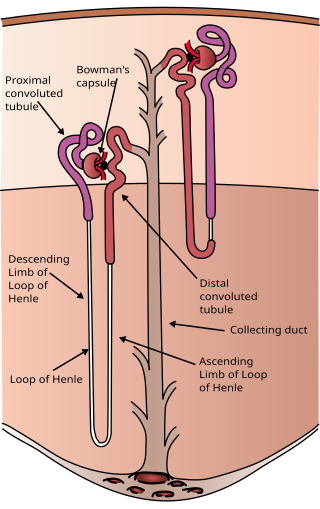
The nephron is the minute or microscopic structural and functional unit of the kidney. It is composed of a renal corpuscle and a renal tubule. The renal corpuscle consists of a tuft of capillaries called a glomerulus and a cup-shaped structure called Bowman's capsule. The renal tubule extends from the capsule. The capsule and tubule are connected and are composed of epithelial cells with a lumen. A healthy adult has 1 to 1.5 million nephrons in each kidney. Blood is filtered as it passes through three layers: the endothelial cells of the capillary wall, its basement membrane, and between the podocyte foot processes of the lining of the capsule. The tubule has adjacent peritubular capillaries that run between the descending and ascending portions of the tubule. As the fluid from the capsule flows down into the tubule, it is processed by the epithelial cells lining the tubule: water is reabsorbed and substances are exchanged ; first with the interstitial fluid outside the tubules, and then into the plasma in the adjacent peritubular capillaries through the endothelial cells lining that capillary. This process regulates the volume of body fluid as well as levels of many body substances. At the end of the tubule, the remaining fluid—urine—exits: it is composed of water, metabolic waste, and toxins.
Diuresis is the excretion of urine, especially when excessive (polyuria). The term collectively denotes the physiologic processes underpinning increased urine production by the kidneys during maintenance of fluid balance.

Uremia is the condition of having high levels of urea in the blood. Urea is one of the primary components of urine. It can be defined as an excess in the blood of amino acid and protein metabolism end products, such as urea and creatinine, which would normally be excreted in the urine. Uremic syndrome can be defined as the terminal clinical manifestation of kidney failure. It is the signs, symptoms and results from laboratory tests which result from inadequate excretory, regulatory, and endocrine function of the kidneys. Both uremia and uremic syndrome have been used interchangeably to denote a very high plasma urea concentration that is the result of renal failure. The former denotation will be used for the rest of the article.

Renal functions include maintaining an acid–base balance; regulating fluid balance; regulating sodium, potassium, and other electrolytes; clearing toxins; absorption of glucose, amino acids, and other small molecules; regulation of blood pressure; production of various hormones, such as erythropoietin; and activation of vitamin D.

Renal physiology is the study of the physiology of the kidney. This encompasses all functions of the kidney, including maintenance of acid-base balance; regulation of fluid balance; regulation of sodium, potassium, and other electrolytes; clearance of toxins; absorption of glucose, amino acids, and other small molecules; regulation of blood pressure; production of various hormones, such as erythropoietin; and activation of vitamin D.

Assessment of kidney function occurs in different ways, using the presence of symptoms and signs, as well as measurements using urine tests, blood tests, and medical imaging.

ADME is the four-letter abbreviation (acronym) for absorption, distribution, metabolism, and excretion, and is mainly used in fields such as pharmacokinetics and pharmacology. The four letter stands for descriptors quantifying how a given drug interacts within body over time. The term ADME was first introduced in the 1960s, and has become a standard term widely used in scientific literature, teaching, drug regulations, and clinical practice.

Glycosuria is the excretion of glucose into the urine. Ordinarily, urine contains no glucose because the kidneys are able to reabsorb all of the filtered glucose from the tubular fluid back into the bloodstream. Glycosuria is nearly always caused by an elevated blood sugar level, most commonly due to untreated diabetes. Rarely, glycosuria is due to an intrinsic problem with glucose reabsorption within the kidneys, producing a condition termed renal glycosuria. Glycosuria leads to excessive water loss into the urine with resultant dehydration, a process called osmotic diuresis.

Glucuronic acid is a uronic acid that was first isolated from urine. It is found in many gums such as gum arabic, xanthan, and kombucha tea and is important for the metabolism of microorganisms, plants and animals.
In pharmacology, clearance is a pharmacokinetic parameter representing the efficiency of drug elimination. This is the rate of elimination of a substance divided by its concentration. The parameter also indicates the theoretical volume of plasma from which a substance would be completely removed per unit time. Usually, clearance is measured in L/h or mL/min. The quantity reflects the rate of drug elimination divided by plasma concentration. Excretion, on the other hand, is a measurement of the amount of a substance removed from the body per unit time. While clearance and excretion of a substance are related, they are not the same thing. The concept of clearance was described by Thomas Addis, a graduate of the University of Edinburgh Medical School.
Probenecid, also sold under the brand name Probalan, is a medication that increases uric acid excretion in the urine. It is primarily used in treating gout and hyperuricemia.
In medicine, the urea-to-creatinine ratio (UCR), known in the United States as BUN-to-creatinine ratio, is the ratio of the blood levels of urea (BUN) (mmol/L) and creatinine (Cr) (μmol/L). BUN only reflects the nitrogen content of urea and urea measurement reflects the whole of the molecule, urea is just over twice BUN. In the United States, both quantities are given in mg/dL The ratio may be used to determine the cause of acute kidney injury or dehydration.
The fractional excretion of sodium (FENa) is the percentage of the sodium filtered by the kidney which is excreted in the urine. It is measured in terms of plasma and urine sodium, rather than by the interpretation of urinary sodium concentration alone, as urinary sodium concentrations can vary with water reabsorption. Therefore, the urinary and plasma concentrations of sodium must be compared to get an accurate picture of kidney clearance. In clinical use, the fractional excretion of sodium can be calculated as part of the evaluation of acute kidney failure in order to determine if hypovolemia or decreased effective circulating plasma volume is a contributor to the kidney failure.

Renal compensation is a mechanism by which the kidneys can regulate the plasma pH. It is slower than respiratory compensation, but has a greater ability to restore normal values. Kidneys maintain the acid-base balance through two mechanisms: (1) the secretion of H+ ions into the urine (from the blood) and (2) the reabsorption of bicarbonate HCO−
3 (i.e., bicarbonate moves from urine back into the blood). The regulation of H+ ions and bicarbonate HCO−
3 is determined by the concentration of the two released within the urine. These mechanisms of secretion and reabsorption balance the pH of the bloodstream. A restored acid-base balanced bloodstream thus leads to a restored acid-base balance throughout the entire body.

Phenylacetylglutamine is a product formed by the conjugation of phenylacetate and glutamine. It is a common metabolite that occurs naturally in human urine.
Osmoregulation is the active regulation of the osmotic pressure of an organism's body fluids, detected by osmoreceptors, to maintain the homeostasis of the organism's water content; that is, it maintains the fluid balance and the concentration of electrolytes to keep the body fluids from becoming too diluted or concentrated. Osmotic pressure is a measure of the tendency of water to move into one solution from another by osmosis. The higher the osmotic pressure of a solution, the more water tends to move into it. Pressure must be exerted on the hypertonic side of a selectively permeable membrane to prevent diffusion of water by osmosis from the side containing pure water.
For elimination via bile please see: Estimation of Biliary Excretion of Foreign Compounds Using Properties of Molecular Structure. 2014. Sharifi M., Ghafourian T. AAPS J. 16(1) 65–78.