 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Trobalt, Potiga |
| Other names | D-23129, ezogabine (USAN US) |
| AHFS/Drugs.com | Professional Drug Facts |
| MedlinePlus | a612028 |
| License data | |
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 60% |
| Protein binding | 60–80% |
| Metabolism | Liver glucuronidation and acetylation. CYP not involved |
| Elimination half-life | 8 hours (mean), range: 7–11 hours [1] |
| Excretion | Kidney (84%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.158.123 |
| Chemical and physical data | |
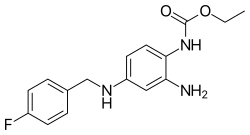
| Formula | C16H18FN3O2 |
| Molar mass | 303.337 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
Retigabine (INN) or ezogabine (USAN) is an anticonvulsant used as an adjunctive treatment for partial epilepsies in treatment-experienced adult patients. [2] The drug was developed by Valeant Pharmaceuticals and GlaxoSmithKline. It was approved by the European Medicines Agency under the trade name Trobalt on March 28, 2011, and by the United States Food and Drug Administration (FDA), under the trade name Potiga, on June 10, 2011. Production was discontinued in June 2017. [3] [4]
Contents
- Adverse effects
- Interactions
- Pharmacology
- Mechanism of action
- Pharmacokinetics
- History
- Clinical trials
- Regulatory approval
- Name
- References
- Further reading
Retigabine works primarily as a potassium channel opener—that is, by activating a certain family of voltage-gated potassium channels in the brain. [5] [6] [7] This mechanism of action is unique among antiepileptic drugs, and may hold promise for the treatment of other neurologic conditions, including tinnitus, migraine and neuropathic pain. The manufacturer withdrew retigabine from clinical use in 2017.